Percutaneous coronary intervention inefficacious in improving severe ischemic left ventricular dysfunction
1. For patients with severe ischemic left ventricular systolic dysfunction on optimal medical therapy, percutaneous coronary intervention (PCI) did not result in additional reductions in mortality and hospitalization.
2. Although quality-of-life scores were higher in those receiving PCI than those on optimal medical therapy alone, this difference narrowed by 24 months.
Evidence Rating Level: 1 (Excellent)
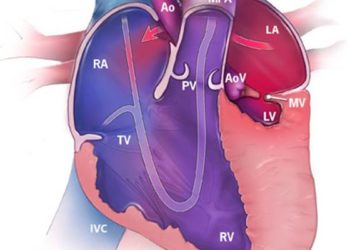
Study Rundown: Coronary artery disease is the chief cause of heart failure. Coronary-artery bypass grafting (CABG) has been shown to improve systolic function in patients with severe ischemic left ventricular dysfunction, resulting in survival benefits, when compared to medical therapy alone. Nevertheless, surgical risks associated with CABG could impact the overall benefit gained in these patients. Therefore, there is a need to investigate PCI revascularization and whether it could improve patient outcomes without CABG-associated hazards. The current study was a randomized, open-label trial assessing PCI as an addition to optimal medical therapy for patients with severe ischemic left ventricular systolic dysfunction. It was found at six and 12 months that PCI did not lower the rates of all-cause mortality and hospitalization for heart failure. Quality-of-life scores were higher in the PCI group at six and 12 months, but this difference narrowed at 24 months. Although the trial was underpowered for the primary outcome, statistical findings suggested that the risk of type II error was low. Thus, the study provided early evidence that PCI did not reduce mortality and hospitalization rates among patients with severe ischemic left ventricular systolic dysfunction, beyond what was achieved by optimal medical therapy alone.
Click here to read the study in NEJM
Relevant Reading: Initial Invasive or Conservative Strategy for Stable Coronary Disease
In-Depth [randomized controlled trial]: The current study was a multicenter, randomized, open-label trial investigating whether revascularization by PCI can benefit patients with severe ischemic left ventricular dysfunction. Patients with a left ventricular ejection fraction (LVEF) of 35% or less, extensive coronary artery disease amenable to PCI, and measurable myocardial viability. Exclusion criteria were a recent acute myocardial infarction, acute decompensated heart failure, or sustained ventricular arrhythmias. Overall, 700 patients were randomized 1:1 to receive either optimal medical therapy alone, which involved individually adjusted pharmacologic and device therapies, or optimal medical therapy with PCI. The primary outcome was the composite of death from any cause or hospitalization for heart failure over a minimum of 24 months. Secondary outcomes included LVEF at six and 12 months, determined through echocardiography, and quality of life (assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ)). The median follow-up was 41 months. Over this time, the primary outcome occurred in 129 (37.2%) of 347 patients in the PCI and 134 (38.0%) of 353 patients in the optimal-medical-therapy group (hazard ratio, 0.99; 95% confidence interval [CI], 0.78-1.27; p=0.96). No statistically significant differences were observed in each component of the primary outcome. The LVEF was also comparable between the groups at 6 months (mean difference, -1.6 percentage points; 95% CI, -3.7-0.5) and 12 months (mean difference, 0.9 percentage points; 95% CI, -1.7-3.4). Lastly, although the PCI group saw higher KCCQ scores than the optimal-medical-therapy group at six and 12 months, this difference diminished at 24 months. The study provided evidence that PCI did not reduce the risk of death from any cause or hospitalization for heart failure in patients with severe ischemic left ventricular systolic dysfunction beyond optimal medical therapy.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.