Perioperative dexmedetomidine decreases the incidence of select complications following kidney transplantation
1. This randomized controlled trial found that giving dexmedetomidine for 24 hours at the time of kidney transplant receipt reduced the incidence of delayed graft function (DGF) following donation-after-cardiac death kidney transplantation.
Level of Evidence Rating: 1 (Excellent)
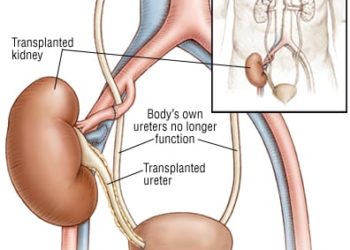
Study Rundown: End stage kidney disease is a significant public health issue and accounts for a growing proportion of patients on dialysis.. Donation after cardiac death (DCD) kidney transplantation provides one solution to this issue although DCD kidneys may be fraught with more complications than one from a living donor including delayed graft function (DGF). Dexmedetomidine is a selective alpha-agonist which acts centrally to produce analgesic, sedative and anxiolytic effects; it is used extensively in intensive care settings and is additionally thought to be renoprotective. The present randomized controlled trial sought to determine whether giving dexmedetomidine perioperatively reduces the risk of complications in patients receiving DCD kidney transplants. 114 patients were randomized to participate in this trial with 56 in the dexmedetomidine group and 54 in the control group. The study drug or placebo was infused at a rate of 0.4ug/kg/h beginning immediately after anesthesia induction and continuing for 24 hours. Median creatinine clearance was higher postoperatively in the dexmedetomidine group compared to the control group on postoperative days 1 and 2. DGF occurred in approximately 18% of the patients in the dexmedetomidine group and 34% of those in the control group. Kaplan-Meier analysis revealed that the risk of DGF in the dexmedetomidine group was significantly lower than the control group. The study drug was also found to reduce the risk of acute transplant rejection and need for dialysis within one month compared to the control group. The present trial by Xi-Sheng et al found that perioperative infusion of dexmedetomidine for 24 hours in patients receiving a DCD kidney transplantation for end stage renal disease were, to some degree, protected from DGF as well as other complications in the acute postoperative period. Kidney transplantation remains a high-risk procedure and further research to optimize surgical success remains critical. A major highlight of this study is the use of a triple-blinded randomized controlled trial design which effectively reduces risk of bias. Some trial limitations include the small sample size and highly-controlled study procedures, which may limit the generalizability of these findings. Certainly, a larger international trial of this intervention is warranted as Xi-Sheng et al demonstrated the promising role that dexmedetomidine can play in reducing risk of complications in DCD kidney transplantation.
Click here to read this study in JAMA Network Open
Relevant reading: Early graft loss after kidney transplantation: risk factors and consequences
In-Depth [randomized clinical study]: This study is a randomized controlled trial conducted in China. Donor kidneys were harvested following cardiac death as evidenced by a positive apnea test. Standard procedures and guidelines for organ harvest and transplantation were followed for the purposes of this trial. Recipients were adults with end stage kidney disease who were currently on dialysis and scheduled to receive a DCD kidney; patients with cardiac disease were excluded. Patients were randomized in a 1:1, block-based fashion to receive either dexmedetomidine or normal saline (placebo); this study was triple-blinded. The primary outcome of DGF was defined by the need for dialysis during the first week postoperatively. All patients were treated by the same team of healthcare workers to manage perioperative factors (i.e., medications, intake, immunosuppressants, etc.) to standardize trial data as best as possible. Operative factors such as mean anastomosis time and length of stay in hospital were comparable between the two groups. Difference in median creatinine clearance between the experimental and control group was 2.0 (95% confidence interval 0.5-6.8ml/min; 9.9 [interquartile range 4.9-21.2] mL/min for dexmedetomidine vs 7.9 [2.0-10.4] mL/min for normal saline) on postoperative day 1 and was 15.0 (0.4-18.5ml/min; 29.6 [9.7-67.4] mL/min vs 14.6 [3.8-45.1]) on postoperative day 2. The primary outcome occurred in 17.9% of the experimental group patients and 34.5% of those in the control group; the odds ratio for DGF was 0.41 (95% confidence interval 0.17-0.98) in favor of dexmedetomidine. The hazard ratio for DGF was 0.48 (0.23-0.99) in the dexmedetomidine versus control group. Analysis of secondary outcomes revealed that dexmedetomidine reduced the need for dialysis within 30 days of surgery (1.8% vs. 5.5% in the control group) and acute, biopsy-proven rejection (8.9% vs. 12.7%) compared to the control group.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.





![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-75x75.jpg)