Physical activity is associated with a reduction in all-cause mortality in patients with newly diagnosed Parkinson Disease
1. Newly diagnosed Parkinson Disease patients who were active had an associated reduced all-cause mortality compared to those who were inactive.
2. Activity of any intensity level was associated with reduced mortality, with progressively greatest reduction at longer and more intense (greater metabolic equivalents) activity.
Evidence Rating Level: 2 (Good)
Study Rundown: There are few disease-modifying treatments for Parkinson Disease (PD) currently supported by evidence. Physical activity (PA) has been associated with decreasing the risk of development or progression of PD. Thus, PA may be a potential disease-modifying therapeutic option for PD. This study evaluated whether PA decreased all-cause mortality of PD patients. Data on demographics and PD diagnosis were taken from the Korean National Health Insurance Service (NHIS) database. PA was collected from a 7-day recall and reported as total metabolic equivalent of task (MET) minutes/week, where 3, 5, and 8 METs were light, moderate, and intense exercise. 10,699 PD patients (54% women, 46% men, age = 69.2±8.8 years) were followed for 4.5±1.4 years. Increased mortality was associated with higher age, being male, high BMI, high disability, and comorbidities. Participants who died had, on average, less PA than those who did not. PD patients who were active had an associated reduced mortality compared to those who were inactive. Activity of any intensity reduced mortality, with longer and greater METs progressively reducing mortality. One limitation of this study is the high potential for selection bias for participants with health-seeking behaviours given the inclusion criteria of having regular health checkups to assess PA. Given the 7-day recall sampling of PA, recall bias could exist. Additionally, there could be sampling error if the 7-day recall weeks were not representative of the individuals’ PA. Finally, subtypes of PD symptoms, anti-PD medications, and other habits like caffeine consumption, diet, and smoking were not available in this database for analysis or to be removed as potential confounders for their known association with PD and effects on mortality.
Click to read the study in JAMA Neurology
Click to read an accompanying editorial in JAMA Neurology
Relevant Reading: Tai chi and postural stability in patients with Parkinson’s disease
In-Depth [retrospective cohort]: Patients older than 40 with newly diagnosed PD who attended check-ups 2 years before and after diagnosis were identified in the Korean NHIS database. A 7-day recall of PA (type and intensity) is reported in this database at each checkup. These PAs were converted into total MET minutes/week and classified as light, moderate, or intense/vigorous. Patients were then classified as active or inactive if they met a threshold of PA. Vigorous activity included any high-intensity PA like running, fast biking, aerobatics, or climbing for at least 20 minutes; moderate activity included moderate-intensity PA like fast walking, riding a bicycle at a normal speed, and doubles tennis for at least 30 minutes; finally, light activity included any light-intensity PA like walking for at least 30 minutes. Patients were defined as physically active if they completed at least 3 days of intense or at least 5 days of light PA. Of the 10,699 participants, those who died were more likely to be older (73.2±7.5 years vs 68.3±8.8 years; P < 0.001). Women were more likely to be among those who did not die compared to those who did (39.6% vs 56.9%; P < 0.001). Increased mortality was associated with higher age (HR = 1.07, 95%CI = 1.06-1.07; P < 0.001), disability (HR = 1.92, 95% CI = 1.66-2.23; P < 0.001), and Charlson Comorbidity Index (HR = 1.13, 95% CI = 1.11-1.16; P < 0.001). Decreased mortality was associated with female sex (HR = 0.53, 95% CI = 0.48-0.58; P < 0.001) and BMI (HR, 0.94, 95% CI = 0.92-0.95; P < 0.001). The average participant who died performed 270 MET-minutes/week of PA, while those who did not performed 450 MET-minutes/week. Patients with PD who were physically active compared to inactive had an associated reduced mortality by log-rank test (P < 0.001). The risk of death for PD patients was reduced for all PA levels (vigorous: HR = 0.80, 95% CI = 0.69-0.93; moderate-intensity: HR = 0.66, 95% CI = 0.55-0.78; light-intensity: HR = 0.81, 95% CI = 0.73-0.90). PD patients in the first compared to the fourth quartile range had progressively decreasing risk of mortality (HR = 0.61, 95% CI = 0.53-0.70; P < 0.001). Those active before and after PD diagnosis had the greatest mortality rate reduction compared to those who were always inactive (vigorous: HR = 0.66, 95% CI = 0.50-0.88; moderate: HR = 0.49, 95% CI = 0.32-0.75; light: HR = 0.76, 95% CI = 0.66-0.89). Individuals who became active when they were diagnosed experienced a mortality reduction (vigorous: HR = 0.82, 95% CI = 0.70-0.97; moderate: HR = 0.69, 95% CI = 0.57-0.83; light: HR = 0.86, 95% CI = 0.78-0.98), while those who became inactive had similar mortality rates to those who were always inactive.
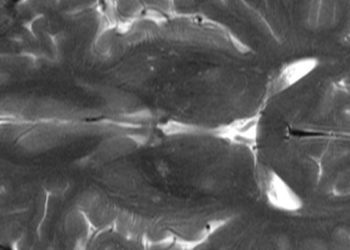
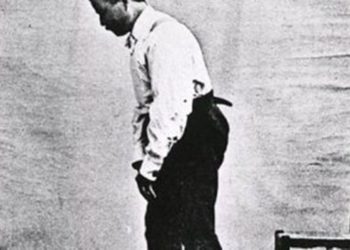
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.