Physical therapy equal to surgery for symptomatic meniscal tears
[tabs tab1=”2MM Rundown” tab2= “2MM Full Report”]
[tab]
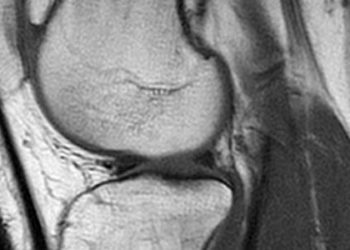
Image: PD
1. In patients over 45 with a symptomatic meniscal tear and mild to moderate osteoarthritis (OA), physical therapy (PT) may provide equal functional improvement to surgery.
2. Arthroscopic partial meniscectomy (APM) and physical therapy each provide enhanced functional and pain outcomes for patients with symptomatic meniscal tears.
For patients over the age of 45 with a symptomatic meniscal tear and concomitant mild to moderate OA, PT may provide equal functional outcomes to APM. While generalization of these findings should be made with caution, this study does serve to reinforce that both PT and APM enhance functionality in patients with meniscal tears and OA. It also provides reassurance that PT is a sensible option in cases where surgical intervention must be delayed.
Several limitations of this study are inherent to any surgical vs, non-surgical trial. They include patient preference, surgeon equipoise, and a lack of blinding. Additionally, 30% of the patients randomized to the PT group crossed-over to the APM group by six months, which may have artificially inflated the positive outcomes seen in the PT group. Although vulnerable to bias, a subgroup analysis of patients that did not cross-over between groups also suggested an enhanced benefit for APM the WOMAC scale.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
[/tab]
[tab]
Image: PD
1. In patients over 45 with a symptomatic meniscal tear and mild to moderate osteoarthritis (OA), physical therapy (PT) may provide equal functional improvement to surgery.
2. Arthroscopic partial meniscectomy (APM) and physical therapy each provide enhanced functional and pain outcomes for patients with symptomatic meniscal tears.
This [multicenter, randomized ] study included 351 patients 45 years of age or older with a symptomatic meniscal tears and concomitant mild to moderate osteoarthritis (OA). OA was detected on MRI and/or plain radiograph and graded on the Kellgren-Lawrence scale of osteo-arthrosis. Subjects were randomized to receive either immediate arthroscopic partial meniscectomy (APM) and standard post-operative physical therapy (PT) or conservative management with PT only. APM involves trimming the damaged meniscus back to a stable rim. Patient outcomes were assessed via the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) as well as the Knee Injury and Osteoarthritis Outcome Scale (KOOS) and SF-36 obtained at baseline and 3, 6, and 12 months.
Employing an intent-to-treat analysis, at six months the mean improvement in WOMAC scores for the APM group was 20.9 points as compared to 18.5 points in the PT group. KOOS pain scores showed similar proximity with the APM group at 24.2 points versus 21.3 points in the PT group. By six months, 50 patients randomized to the PT group had undergone surgery. Conversely, 9 patients randomized to surgery decided not to have it. In a subgroup analysis of patients that did not crossover, 67% of patients who had APM had improvement of at least 8 points on the WOMAC scale as compared to just 44% of those treated with PT alone.
In sum: For patients over the age of 45 with a symptomatic meniscal tear and concomitant mild to moderate OA, PT may provide equal functional outcomes to APM. While generalization of these findings should be made with caution, this study does serve to reinforce that both PT and APM enhance functionality in patients with meniscal tears and OA. It also provides reassurance that PT is a sensible option in cases where surgical intervention must be delayed.
Several limitations of this study are inherent to any surgical vs non-surgical trial. They include patient preference, surgeon equipoise, and a lack of blinding. Additionally, 30% of the patients randomized to the PT group crossed-over to the APM group by six months, which may have artificially inflated the positive outcomes seen in the PT group. Although vulnerable to bias, a subgroup analysis of patients that did not cross-over between groups also suggested an enhanced benefit for APM the WOMAC scale.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
By Chaz Carrier and Allen Ho
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.
[/tab]
[/tabs]