Point-of-care hemostatic test during TAVR procedure may help predict negative outcomes
1. Closure time with adenosine diphosphate (CT-ADP) measurement after a transcatheter aortic-valve replacement (TAVR) procedure was predictive of patients with paravalvular aortic regurgitation.
2. Elevated CT-ADP times were more predictive of patient death 1 year post-TAVR than aortic or mitral regurgitation.
Evidence Rating: 1 (Excellent)
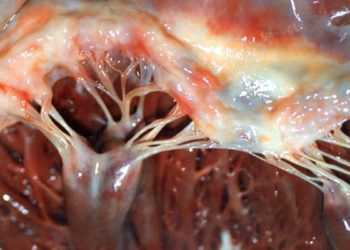
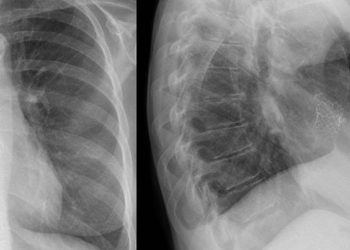
Study Rundown: Following a TAVR for treatment of aortic regurgitation 10-20% of patients have residual aortic regurgitation, likely due to paravalvular leak. Patients with residual aortic regurgitation are at increased risk of negative outcomes, including death and rehospitalization. Evaluating patients for residual aortic regurgitation after a TAVR and correcting the issue while in the catheterization lab with greater accuracy is a currently unmet clinical need.
This study sought to evaluate how the point-of-care hemostatic CT-ADP test, which is highly sensitive to von Willebrand factor (vWF) deficits observed in patients with aortic stenosis or valvular regurgitation, could be used for screening patients for aortic regurgitation post-TAVR. Blood samples used for CT-ADP testing were taken at 1 point before the TAVR and 3 points after the procedure. CT-ADP times and deficits in vWF were assessed and compared to a patient’s clinical state (having aortic regurgitation or not as determined by transesophageal echocardiography (TEE)). Patients were additionally followed for 1 year after their TAVR, and outcomes of death and stroke were tracked and assessed against various predictive markers including CT-ADP values. Results showed CT-ADP values were predictive of residual aortic regurgitation at various intraoperative time points. CT-ADP and vWF values were also more predictive of 1-year mortality than TEE, suggesting a biomarker potentially more useful for predicting long term outcomes than traditional imaging.
Click to read the study, published today in NEJM
Relevant Reading: von Willebrand Factor as a Biological Sensor of Blood Flow to Monitor Percutaneous Aortic Valve Interventions
In-Depth [prospective cohort]: This study took place from August 2012 to April 2014 at 3 hospitals in France. The cohort included 183 patients undergoing a TAVR. Patients were imaged by TEE after the TAVR, and again after a valve dilation or implantation of an additional valve (48 of 183 patients) if their initial TEE suggested aortic regurgitation. Blood samples were collected before the procedure and 3 times during the procedure to evaluate how von Willebrand factor and CT-ADP values changed for patients.
Patients were also followed up for 1 year after their procedure for assessment of stoke or death. Of the patients studied, 137/183 had no regurgitation after the TAVR, 20/183 had regurgitation that was corrected in the cath lab, and 26/183 had persistent regurgitation. Patients with residual regurgitation had von Willebrand factor deficiencies and CT-ADP values significantly different (p < 0.001) from those without regurgitation at the end of the procedure. At the end of the procedure CT-ADP values for patients with no regurgitation were 45% lower than baseline, and patients with corrected regurgitation had CT-ADP values 44% lower than before regurgitation correction. Patients with persistent regurgitation had elevated CT-ADP values at all 4 sampled times. Receiver-Operating-Characteristic area under the curve analysis suggested a threshold value of 180 seconds to determine elevated (low von Willebrand factor, high risk) vs. non-elevated values. This value had sensitivity, specificity, and negative predictive values of 92.3%, 92.4%, and 98.6%, respectively for discriminating patients with aortic regurgitation or without at the 4th sampling point. For long term follow-up, patients with an elevated CT-ADP value (180+ seconds) had a 3.5 times increased risk of death at 1 year compared to those with a CT-ADP less than 180 seconds (p < 0.001). Additionally, an elevated CT-ADP was a better predictor of mortality than aortic regurgitation as seen on TEE or mitral regurgitation at baseline. Overall, CT-ADP may have potential to be a useful biomarker to assessing patients that may be at increased risk for adverse outcome after an initial TAVR, allowing both short term interventions (paravalvular regurgitation fix) and long term attention.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.