Prednisolone vs placebo in severe alcoholic hepatitis [Classics Series]
1. Compared to placebo, treating patients with severe alcoholic hepatitis with 28 days of prednisolone significantly improved the short-term survival up to 6 months.
2. There remains significant controversy surrounding the use of glucocorticoids in managing severe alcoholic hepatitis, as numerous other trials have demonstrated no mortality benefit, but significantly higher risk of infection with glucocorticoid therapy.
Original Date of Publication: February 1992
Study Rundown: Alcoholic hepatitis is a form of acute liver disease that may develop in individuals with prolonged, heavy alcohol intake. In patients with alcoholic hepatitis, conventional management consists of abstinence from alcohol, correction of dietary deficiencies, and supportive care. Maddrey discriminant function is a prognostic tool that is used to assess the severity of alcoholic hepatitis. Patients with scores ≥32 are termed severe alcoholic hepatitis, and experience significantly higher rates of morbidity and mortality than those with less severe disease. Prior to this study, several randomized trials had explored using glucocorticoids in managing alcoholic hepatitis, though results were conflicting. Meta-analyses of these trials suggested that there may be a benefit of using glucocorticoids in patients with severe disease. Thus, the purpose of this trial was to determine whether treating patients with severe alcoholic hepatitis with glucocorticoids would significantly reduce mortality as compared with placebo. In summary, corticosteroid therapy was found to significantly reduce mortality in patients with severe alcoholic hepatitis, as characterized by Maddrey discriminant function ≥32 or hepatic encephalopathy. Subsequent studies of glucocorticoids have continued to produce conflicting results, and there remains controversy surrounding their use in managing alcoholic hepatitis, as other studies have demonstrated significantly higher rates of infection with prednisolone therapy. While pentoxifylline has also been studied in severe alcoholic hepatitis, the results describing their effects have also been conflicting.
Click to read the study in NEJM
In-Depth [randomized controlled study]: A total of 65 participants were selected from 2 hospitals in France and randomized to treatment with prednisolone 40 mg daily or placebo for 28 days. Patients unable to take oral medications received intravenous infusions of prednisolone or placebo. Patients were eligible for the trial if they had biopsy-proven alcoholic hepatitis and severe alcoholic hepatitis (i.e., spontaneous hepatic encephalopathy or Maddrey discriminant score ≥32). Exclusion criteria included gastrointestinal bleeding or bacterial infection that could not effectively be treated within the first 48 hours. The primary endpoint was mortality within 2 months.
The two groups did not differ with regards to sex, age, duration of hospitalization before entry into the study, the presence of ascities, spontaneous hepatic encephalopathy, or esophageal varices. Survival in the prednisolone group was 88±5% and 88±5% at 1 and 2 months, respectively, compared to 62±9% and 45±8% in the placebo group for the same timepoints. Survival was significantly better in patients treated with corticosteroid than those taking placebo, regardless of the presence or absence of encephalopathy (adjusted log-rank test 9.9; p = 0.0017). The cumulative six-month survival rates were 84±6% in the prednisolone group and 45±9% in the placebo group (low-rank test 9.5; p = 0.002).
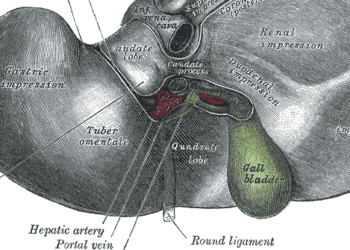
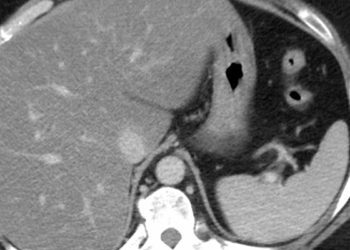
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.