Prenatal iron supplementation not linked to placental malaria risk
1. Prenatal iron supplementation was not associated with increased risk of placental malaria in a malarial endemic region.
2. Iron supplementation was associated with a significantly reduced risk of maternal anemia at time of delivery compared with placebo.
Evidence Rating Level: 1 (Excellent)
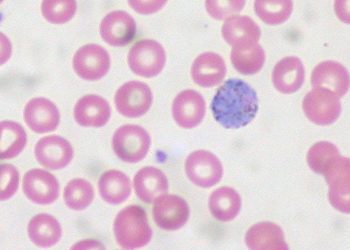
Study Rundown: Anemia is a common problem in pregnancy, and while there is a physiologic anemia of pregnancy, more severe anemia in pregnancy is associated with increased rates of adverse maternal and neonatal health outcomes. In some areas of the developing world like sub-Saharan Africa, iron deficiency is a leading cause of maternal and neonatal morbidity. The World Health Organization currently recommends iron supplementation for all pregnant women living in areas with high anemia prevalence. However, recent studies in children suggest that in malaria endemic regions, iron supplementation may facilitate spread of infection by providing an increased nutrient source for host pathogens. There is currently little data comparing the risk of malarial acquisition related to iron supplementation in pregnant women in areas with high malaria burden. In this double-blind, randomized clinical trial, researchers assessed pregnancy outcomes in iron-replete, nonanemic pregnant women in a malaria endemic region of Tanzania who received either daily iron supplementation or placebo.
Findings demonstrate that daily iron supplementation was not associated with an increased risk of placental malaria or other adverse events. Compared with placebo, women taking iron supplements had a significantly reduced risk of anemia and an improved iron status at delivery. Strengths of this study included a rigorous design and large sample size. One limitation was the low overall risk of malaria in the study population due to the distribution of malaria prophylaxis and widespread malaria control practices. Therefore, findings may not be applicable in regions with poor malaria control. Risk-benefit studies in areas with poor malaria control would provide additional insight.
Click to read the study in JAMA Pediatrics
In-Depth [randomized controlled trial]: Researchers randomized iron-replete, nonanemic, pregnant women presenting for antenatal care in the malaria endemic region of Dar es Salaam, Tanzania to receive 60 mg of daily iron (n = 750) or placebo (n = 750). Participants were followed every 4 weeks for standard prenatal care, including malaria screening and prophylaxis. Primary outcomes included placental malaria and maternal hemoglobin level at delivery and birth weight.
Compared to placebo, pregnant women randomized to iron supplements did not experience increased risk of placental malaria (RR = 1.03, 95%CI 0.65-1.65) and delivered neonates of similar birth weights (3155 vs. 3137 g, p = 0.89). Iron supplementation was associated with greater increase in hemoglobin from enrollment to delivery (0.1 vs. -0.7, p < 0.001) and decreased risk of anemia at delivery (RR = 0.60, 95%CI 0.51-0.71). Over 90% of the study population used malaria control measures.
Image: CC/Wiki/Alan R Walker
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.