Prescription of antibiotics on wards associated with Clostridium difficile infection
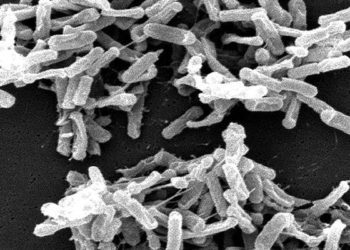
1. Clostridium difficile (C. difficile) infection is often seen in hospitalized patients who take antibiotics.
2. Antibiotic prescribing patterns on the ward-wide level were associated with incidence of C. difficile infection.
Evidence Rating Level: 2 (Good)
Study Rundown: Clostridium difficile is a bacterium that produces copious watery diarrhea, and is notorious as a scourge affecting hospitalized patients. On an individual level, research has shown that inpatients taking antibiotics are 60% more likely to develop a C. difficile infection, particularly if they are taking clindamycin, cephalosporins, or fluoroquinolones. This study sought to investigate C. difficile infection rates on the level of different wards in a hospital, in the acute care setting. The authors hypothesized that ward prescription patterns affected patient susceptibility to infection beyond, and independent of, the risk of taking antibiotics on an individual level.
The primary outcome was the incidence of hospital-acquired C. difficile infection. In this retrospective cohort, the investigators found that after adjusting for potential confounders, there was a 1.34-fold increase in C. difficile infection rate for each 10% increase in days of ward antibiotic exposure. The investigators excluded patients in psychiatry, obstetrics, neonatal, and long-term care wards, as previous studies have suggested that the pretest probability of C. difficile infection is lower compared to that in acute care wards. Strengths of the study include a fairly large number of patients enrolled. Limitations of the study include the retrospective nature, as well as the single-center enrollment, which may limit generalizability to other populations.
Click to read the study, published today in JAMA Internal Medicine
In-Depth [retrospective cohort]: The cohort in this study consisted of 34,298 adult patients without a previous C. difficile infection, hospitalized at a large teaching hospital in Toronto, Canada, between 2010 and 2014. C. difficile infections were identified via active surveillance, and defined as a positive toxin PCR combined with either diarrhea (consisting of three or more watery stools during 24 hours), or identification of pseudomembranes on endoscopy or histopathology. Pharmacy records were obtained to investigate antibiotic exposures, and both patient risk factors, such as age, sex and number of previous admissions, and ward-level risk factors such as hand hygiene adherence were measured.
255 patients developed new-onset C. difficile infection during the study period (5.95 per 10,000 patient-days; 95% CI 5.26-6.73). Age, readmission, direct exposure to antibiotics, and use of a feeding tube were individual characteristics associated with increased risk of infection. At the ward-level, days of antibiotic use was the strongest predictor of infection. A 10% increase in ward-level antibiotic use was associated with an increased incidence of infection of 2.1 per 10,000 patient-days (P<.001) when individual patient risk factors were not accounted for, and a 1.34 increased risk (95% CI 1.16-1.57) when these factors were adjusted for.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.