Preventive angioplasty reduces adverse cardiac events in patients with non-flow-limiting vulnerable plaques
1. Patients in the PCI group reported significantly lower rates of cardiac death, revascularization, and hospitalization than those in the medical therapy alone group.
2. Serious clinical or adverse events were comparable in both groups.
Evidence Rating Level: 1 (Excellent)
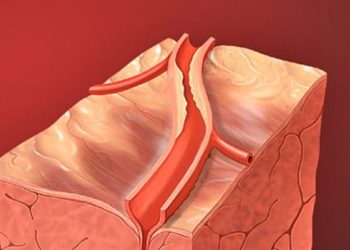
Study Rundown: Acute coronary syndrome and sudden cardiac death may occur from the rupture of lipid-rich atherosclerotic plaques. While the risk of plaque rupture and thrombosis is well known, many of these plaques have not progressed enough to limit flow. As such, whether preventative percutaneous coronary intervention (PCI) for patients with such plaques is beneficial is not well understood. This randomized controlled trial aimed to evaluate whether medical therapy and preventive PCI of non-flow-limiting vulnerable plaques improves clinical outcomes compared to medical therapy alone. The primary outcome of this study was a composite of cardiac death, target-vessel myocardial infarction (MI), target-vessel revascularization, and hospitalization for unstable angina at 2 years, while the key secondary outcome was the occurrence of serious clinical or adverse events. The study found that preventive PCI significantly reduced major adverse cardiac events compared to medical therapy alone without significantly increasing adverse events. Although this study was well done, it was limited by its open-label design and the potential for unmeasured confounders.
Click to read the study in The Lancet
Relevant Reading: Complete Revascularization with Multivessel PCI for Myocardial Infarction
In-depth [randomized controlled trial]: Between Sept 23, 2015, and Sept 29, 2021, 5627 patients were screened for eligibility across 15 research hospitals in 4 countries. Included were patients ≥18 years old with non-flow-limiting vulnerable coronary plaques. Altogether, 1606 patients (803 in PCI plus medical therapy and 803 in medical therapy alone) were included in the final analysis. The composite outcome of cardiac death, target-vessel MI, target-vessel revascularization, and hospitalization for unstable angina occurred in significantly fewer patients in the PCI group compared to the medical therapy alone (0.4% vs. 3.4%, 95% confidence interval [CI] -4.4 to -1.8, p=0.0003). Serious clinical or adverse events did not differ between the PCI and medical therapy groups (0.5% vs. 1.3%, 95% CI -1.7 to 0.2 for death; 1.1% vs. 1.7%, 95% CI -1.7 to 0.6 for MI). Findings from this study suggest that preventive PCI reduces major adverse cardiac events in patients with non-flow-limiting vulnerable coronary plaques.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.