Radiofrequency Ablation vs Stereotactic Body Radiotherapy for Recurrent HCC
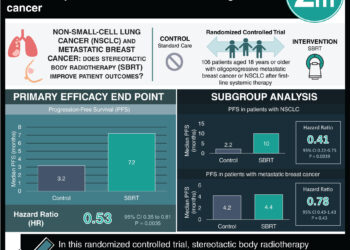
1. Local progression-free survival at 3 years was 84.3% in the SBRT group vs 67.3% in the RFA group, with HR 0.45 (significant).
2. HR for progression-free survival (HR 0.76) and overall survival (HR 0.91) was nonsignificant.
Evidence Rating Level: 1 (Excellent)
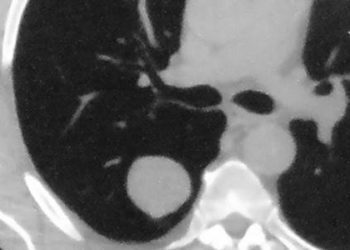
Study Rundown: Radiofrequency ablation (RFA), an effective and routine treatment for both primary and recurrent hepatocellular carcinoma (HCC), has prompted the exploration of alternatives like stereotactic body radiotherapy (SBRT), which delivers precise high-dose radiation with minimal impact on surrounding tissues. Retrospective studies suggest SBRT offers outcomes comparable to RFA. This study was the first randomized trial assessing RFA vs SBRT for recurrent HCC. The primary endpoint was local progression-free survival (LPFS) and secondary endpoints included progression-free survival (PFS), overall survival (OS), local control rate (LCR), and safety. LPFS at 3 years was 84.3% in the SBRT group vs 67.3% in the RFA group. It was found that the HR for LPFS was HR 0.45 (significant). It was found that SBRT performed better than RFA in LPFS for tumours ≤2 cm (HR 0.39, significant), however, this was not significant for larger (2-5 cm) tumours (HR 0.58, non-significant). LCR at 3 years was 92.8% for SBRT vs 75.9% for RFA with a 3-year OR 0.25 (significant). Median PFS time was 37.6 months for SBRT vs 27.6 months for RFA, with HR 0.76 (non-significant). OS at 3 years was 90.3% for SBRT vs 91.0% for RFA, with HR 0.91 (non-significant). Regarding safety, most adverse events were grade 1-2 with only 1 case of grade 3-4 events in each arm, a pneumothorax in the RFA group and thrombocytopenia in the SBRT group. The strengths of this study included the methodology, and the limitations included the small sample size. Overall, this study found that SBRT has some improved minor outcomes compared to RFA in treating adults with small recurrent HCC.
Click to read the study in JCO
Relevant Reading: Outcomes after stereotactic body radiotherapy or radiofrequency ablation for hepatocellular carcinoma
In-Depth [randomized controlled trial]: This open-label single institution trial was conducted in China and enrolled adults with recurrent small (<5cm) HCC and randomized them (1:1) to either SBRT (n=83) or RFA (n=83). Most patients (88%) had hepatitis B virus (HBV)–related HCC. Some patients received a secondary RFA if residual disease was found after the first RFA. The median radiation dose of the SBRT group was 45 Gy (IQR, 42-48) in three fractions. Median follow-up time was 42.8 (95%CI, 39.8-45.8) months in the SBRT group and 42.9 (95%CI, 40.7-45.1) months in the RFA group. LPFS at 3 years was 84.3% (95%CI, 76.5-93.0) in the SBRT group vs 67.3% (95%CI, 57.6-78.6) in the RFA group. It was found that the HR for LPFS was HR 0.45 (95%CI, 0.24-0.87, p=0.014). It was found that SBRT performed better than RFA in LPFS for tumours ≤2 cm (HR 0.39, 95%CI, 0.17-0.89, p=0.020), however, this was not significant for larger (2-5 cm) tumours (HR 0.58, 95%CI, 0.20-1.68, p=0.310). LCR at 3 years was 92.8% for SBRT vs 75.9% for RFA with a 3-year OR 0.25 (95%CI, 0.09-0.65, p=0.005). Median PFS time was 37.6 (95%CI, 26.0-49.2) months for SBRT vs 27.6 (95%CI, 20.3-34.8) months for RFA, with HR 0.76 (95%CI, 0.50-1.15, p=0.190). OS at 3 years was 90.3% (95%CI, 83.7-97.5) for SBRT vs 91.0% (95%CI, 84.8-97.6) for RFA, with HR 0.91 (95%CI, 0.37-2.22, p=0.830). With regards to safety, most adverse events were grade 1-2 with only 1 case of grade 3-4 events in each arm, a pneumothorax in the RFA group and thrombocytopenia in the SBRT group. Overall, this study found that SBRT has some improved minor outcomes compared to RFA in treating adults with small recurrent HCC.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.


![siRNA against antithrombin alleviates symptoms of hemophilia [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/04/clot-CCWiki-75x75.jpg)

