Rates of postoperative pulmonary complications higher for patients receiving Etomidate vs. Propofol
1. For elderly patients receiving elective abdominal surgery, there was no significant difference in the rate of composite major in-hospital postoperative complications in older patients receiving etomidate or propofol for induction.
2. In patients who received etomidate versus propofol, there was a significantly higher incidence of postoperative pulmonary complications, specifically pneumonia.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The use of etomidate as an intravenous anaesthetic is controversial; its hemodynamic stability is a benefit for induction in high-risk patients, but it can potentially cause adrenal insufficiency postoperatively and has a controversial impact on outcomes, including pneumonia in trauma patients, which causes people to generally favour propofol as an induction agent. There is quite limited evidence for etomidate use in high-risk patients, especially for maintenance anesthesia, and most evidence regarding etomidate focuses on boluses rather than infusions. The Etomidate vs Propofol for In-hospital Complications (EPIC) trial hypothesizes that etomidate for maintenance and induction does not increase in-hospital morbidity after abdominal surgery in older patients versus propofol. The EPIC trial was a multicenter randomized controlled trial in 22 tertiary Chinese hospitals that randomized patients 1:1 to receive etomidate or propofol as intravenous anesthetic. Included were patients aged 65 to 80 undergoing elective abdominal surgery. The primary endpoint of this study was the composite of major in-hospital complications during patient hospital stay including severe cardiovascular, pulmonary, neurologic, gastrointestinal, urological, hematological, infectious, and thromboembolic complications as well as death. In total, 1917 patients were recruited from August 2017 to November 2019, with 967 patients receiving etomidate, and 950 patients receiving propofol. With respect to the primary endpoint, in-hospital major complications occurred in 90 of 967 participants in the there was no significant difference in the primary endpoint between groups (p=.66). There were no significant between-group differences in individual complication types except for pulmonary complications (2.0% vs 0.5%; RD, 1.4%; 95% CI, 0.6%-2.3%; p=.005). Of note, there was a higher incidence of pneumonia in the etomidate group compared to the propofol group (2.0% vs 0.3%; RD, 1.7%; 95% CI, 0.7% to 2.8%; P=.001). Overall, this study suggests that in older patients undergoing total intravenous anesthesia for abdominal surgery, etomidate infusion did not increase composite in-hospital complications when compared to propofol infusion. Given the controversy and lack of evidence surrounding etomidate infusions in older patients, this study was important to explore the use of etomidate, especially with its property of hemodynamic stability when compared to propofol. However, caution should be practiced in patients at a high risk of pulmonary complications, given that the study suggests higher incidence of pulmonary complications, especially pneumonia, in patients that received etomidate. A major limitation of this study is the population; high-risk populations were excluded, which would likely benefit most from etomidate versus propofol given the hemodynamic stability of etomidate. Furthermore, the primary endpoint was major post-operative complications, but clinical significance between events was not reflected in the analysis.
Click to read the study in JAMA Surgery
Relevant Reading: Etomidate increases susceptibility to pneumonia in trauma patients
In-Depth [randomized controlled trial]: The EPIC trial aimed to compare major post-operative in-hospital complications in older patients undergoing total intravenous anesthesia (TIVA) for elective abdominal surgery. Included were patients aged 65 to 80 receiving TIVA for abdominal surgery. Exclusion criteria included but were not limited to American Society of Anesthesiologists (ASA) Physical Status Classification class higher than 3, body mass index (BMI) lower than 18.5 and higher than 29.9, and surgery duration less than one hour or greater than four hours. In total, 1917 patients were included in the study across 22 tertiary Chinese hospitals between August 2017 to November 2019 and were randomized 1:1 in the propofol or etomidate group. 967 patients received TIVA with etomidate, and 950 patients received TIVA with propofol. The major in-hospital complication rate was 90/967 (9.3%) in patients who received etomidate, and 83/950 (8.7%) in patients who received propofol. With respect to the primary endpoint of in-hospital major complications, there was no significant difference between the two groups, other than a higher incidence of pulmonary complications in patients who received etomidate versus propofol (2% vs 0.5%; RD, 1.4%; 95% CI, 0.6-2.3%; p=.005). In particular, there was a higher incidence of pneumonia in the etomidate group when compared to the propofol group (2.0% vs 3.0%; RD, 1.7%; 95% CI, 0.7-2.8%; p=.001). With respect to secondary outcomes. With respect to secondary outcomes, patients in the etomidate group had a higher rate of hypertension (p<.001) but a lower rate of hypotension (p<.001) when compared to patients in the propofol group. In addition, mean cortisol levels and mean aldosterone were significantly lower in the etomidate versus the propofol group at the end of the surgery and on postoperative day 1, but there was no significant difference in corticotropin levels between the two groups at any time. Compared to baseline in the etomidate group, mean cortisol and aldosterone levels were significantly lower at the end of surgery when compared to before the surgery, but returned to baseline levels early on postoperative day 1. Otherwise, there were no significant between-group differences in median time to response to verbal command, median duration of post-anesthesia care unit, or post-operative nausea and vomiting scores. Furthermore, there were no significant differences in mortality rate between the etomidate and propofol groups at 6 and 12 months after the operation. Overall, findings from the EPIC trial suggests the noninferiority of etomidate compared to propofol for TIVA for major in-hospital complications in patients aged 65 to 80 who received abdominal surgery.
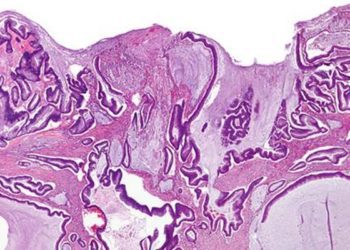
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.