Recognition of kidney allograft microvascular inflammation refines risk stratification for allograft outcomes
1. Patients with a nonrejection-related diagnosis according to the 2019 Banff classification who were reclassified as MVI, DSA-negative, and C4d-negative according to the 2022 Banff classification had worse graft survival than patients with a nonrejection-related diagnosis.
2. Patients with an MVI, DSA-negative, and C4d-negative or probable antibody-mediated rejection had an intermediate cumulative incidence of antibody-mediated rejection compared with patients without a diagnosis of microvascular inflammation and those with active antibody-mediated rejection.
Evidence Rating Level: 2 (Good)
Study Rundown: Kidney transplantation is the treatment of choice for end-stage kidney failure, but allograft rejection continues to be a major cause of long-term allograft loss. The frequent occurrence of graft microvascular inflammation even in the absence of antibody-mediated alloimmune responses highlights our incomplete understanding of the mechanisms underlying these processes. Refinement of the definition of graft microvascular inflammation phenotypes could improve allograft-related precision diagnostics. To address this need, two new phenotypes have been introduced to the 2022 Banff Classification of Renal Allograft Pathology, the accepted standard for diagnosis of kidney allograft rejection: donor-specific antibody-negative and C4d-negative microvascular inflammation and probable antibody-mediated rejection. However, the clinical importance of these new phenotypes remains unclear. The present analysis assessed the implications of the new microvascular inflammation-related phenotypes with respect to allograft outcomes including allograft loss, antibody-mediated rejection, and transplant glomerulopathy. Patients with a nonrejection-related diagnosis according to the 2019 Banff classification who were reclassified as MVI, DSA-negative, and C4d-negative according to the 2022 Banff classification had worse graft survival than patients with a nonrejection-related diagnosis according to both classifications. Limitations of the study included the lack of standardization of immunosuppressive therapy and the lack of systematization of surveillance biopsies following transplantation, which limited analysis of the natural evolution of microvascular inflammation phenotypes and associations between graft outcomes and treatment. Nevertheless, this study provides valuable insights into the prognostic significance of the new microvascular inflammation-related phenotypes of the 2022 Banff classification for pathological assessment of renal allografts.
Click to read the study in NEJM
In-Depth [prospective cohort]: This population-based, multicenter cohort study assessed the clinical relevance of allograft microvascular inflammation in kidney-transplant recipients concerning risk stratification for allograft outcomes. Adult and pediatric kidney-transplant recipients who had undergone at least one kidney-allograft biopsy after transplantation were included. The primary outcomes were microvascular inflammation-related diagnoses as per the 2022 Banff classification and allograft loss. A total of 16,293 biopsy specimens were included in the study and diagnosed according to both the 2019 and 2022 Banff classifications. Of these specimens, 641 were reclassified from a nonrejection-related diagnosis according to the 2019 Banff classification to an MVI, DSA-negative, and C4d-negative or probable antibody-mediated rejection according to the 2022 Banff classification, 76 specimens were reclassified from a diagnosis of T-cell-mediated rejection, and 71 were reclassified from a diagnosis of borderline for acute T-cell-mediated rejection. Patients with a nonrejection-related diagnosis according to the 2019 Banff classification who were reclassified as MVI, DSA-negative, and C4d-negative according to the 2022 Banff classification had worse graft survival than patients with a nonrejection-related diagnosis according to both classifications (hazard ratio, 2.1; 95% Confidence Interval [CI], 1.5 to 3.1). Furthermore, patients with a diagnosis of MVI, DSA-negative, and C4d-negative or probable antibody-mediated rejection had an intermediate cumulative incidence of antibody-mediated rejection compared with patients without a diagnosis of microvascular inflammation and those with active antibody-mediated rejection. The risk of development or progression of transplant glomerulopathy was similar in the MVI, DSA-negative, and C4d-negative groups and the probable antibody-mediated rejection group, and lower in both groups compared to the active antibody-mediated rejection group. In summary, clinical recognition of microvascular inflammation in kidney allografts using the 2022 Banff classification refined risk stratification for allograft outcomes, with patients with microvascular inflammation without evidence of an antibody-mediated cause having an intermediate prognosis compared with patients with antibody-mediated rejection and those with nonrejection.
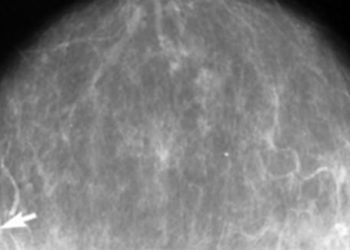
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.