Resection of colorectal liver metastases may improve cost and longevity
1. Surgical resection of colorectal liver metastases was associated with a lower cost (€22,200 vs. €32,800) and increased quality-adjusted life-years (4.02 vs 1.11 years) than non-operative interventions.
2. Median survival was significantly longer in the surgical cohort (41 months) compared to the non-operative group (21 months).
Evidence Rating Level: 2 (Good)
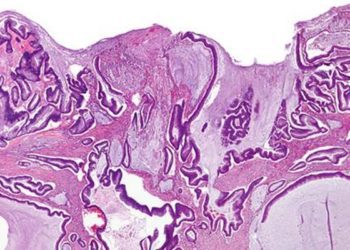
Study Rundown: Colorectal carcinoma remains among the most prevalent and malignant cancers. The liver remains a common site (30-40%) of metastasis, and is associated with poorer survival. Surgical resection of colorectal liver metastases (CRLMs) has been increasingly adopted as standard of care in such patients as the improvement of survival outcomes has been well established; however, no study has analyzed the intervention from a cost standpoint. The authors of this study applied a cost-effectiveness analysis to the surgical resection of CRLMs compared to the non-operative therapeutics for CRLM patients whose disease was never resected. The authors found significantly lower costs associated with surgical resection as well as a significant rise in quality-adjusted life-years (QALY), essentially a measure of the years of “perfect health” associated with each mode of intervention. Such findings are significant in advocating for surgical resection in patients on whom operation is possible given the current climate of financial restraint in the healthcare delivery system. However, there are several limitations inherent to the study design. The study attempted to control for the potentially higher disease burden in the liver of the non-operative cohort by eliminating all patients deemed unresectable due to age/morbidity or presence of metastasis. This does not account for the higher disease burden in the liver itself which precluded resection in these patients and which presumably put them at a higher mortality risk than their operative counterparts. This is likely an unavoidable issue due to the the ethical considerations accompanying a randomized control design given the established survival differences. The study also attempted to incorporate advancements in non-operative therapeutics by comparing the surgical cohort to a more contemporary non-operative group. However, such an adjustment could warrant a comparison to more contemporary surgical cohort given that recent laparoscopic or robotic techniques could incur higher costs.
Click to read the study in the British Journal of Surgery
Relevant Reading: Epidemiology and Management of Liver Metastases From Colorectal Cancer
In-Depth [prospective cohort]: The surgical cohort was comprised of 286 consecutive patients operated for a CRLM between December 1992 and September 2001 at St James’s University Hospital in the UK and followed-up for a minimum of 10 years. The non-operative group was made up of 46 patients presenting with CRLM between January 2008 and January 2010 and were followed until death. Costs were calculated according to the National Health Service (NHS) reference costs. Median survival was 41 months (IQR 17-97) in the operative cohort compared to 21 months (IQR 10-29) in the non-operative group (p 0.001). Cost-utility modeling revealed an average cost of €22,000 and QALY of 4.02 years in the operative cohort, compared to a cost of €32,800 and QALY score of 1.11 in the non-operative group. Sensitivity analysis revealed that the age of the cohort and time horizon did not affect the modeling.
More from this author: Preoperative coagulation status may predict liver transplant complications, Hamstring tendons often regenerate after harvest for ACL repair, Pediatric cardiac surgery occurring at earlier age, with better outcomes over 50+ year review
Image: CC/James Heilman, MD/Wikimedia Commons
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.



![Oxytocin therapy improves social activity in autism mouse model [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/01/Oxytocin-neurophysin-75x75.png)
![Statin therapy does not prevent osteoporotic fractures [JUPITER trial]](https://www.2minutemedicine.com/wp-content/uploads/2014/12/osteoporosis-e1417474828821-75x75.jpg)
![Endostatin directly binds androgen receptors to treat prostate cancer [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/01/Endostatin-75x75.jpeg)