Rezafungin is non-inferior to caspofungin in the treatment of candidemia and invasive candidiasis
1. Global cure was achieved in 59% of the rezafungin group compared to 61% of the caspofungin group.
2. There were no significant differences in the 30-day all-cause mortality and rates of serious adverse events between the two groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Invasive candida infection is associated with high rates of mortality. Emerging resistance to current antifungals necessitates research in to novel treatments. This phase 3 non-inferiority trial evaluating rezafungin versus caspofungin in the treatment of patients with candidemia and invasive candidiasis. The primary outcome was global cure at day 14 and 30-day all-cause mortality. In result, rezafungin was shown to be non-inferior to caspofungin for both primary endpoints. In addition, rezafungin and caspofungin had similar trends of treatment-emergent adverse events and serious adverse events. Limitations of this study include the exclusion of other different forms of invasive candidiasis which could have responding differently to treatment. Nevertheless, this study provides high-quality evidence that supports further investigation of rezafungin as a treatment of candidemia and invasive candidiasis.
Click to read the study in The Lancet
Relevant Reading: Rezafungin: a novel antifungal for the treatment of invasive candidiasis
In-Depth [randomized controlled trial]: ReSTORE was a randomized non-inferiority phase 3 drug trial of intravenous rezafungin versus caspofungin in the treatment of patients candidaemia and invasive candidiasis. Eligible participants were aged 18 years or older, had mycological evidence of candidemia or invasive candidiasis, and were symptomatic. Exclusion criteria included those with prior treatment with more than two days of antifungal therapy, severe liver disease or transaminitis, or presence of an indwelling catheter. Participants were randomized 1:1 to rezafungin (n = 100) or caspofungin (n = 99). Treatment regimen in the rezafungin group was 400 mg rezafungin IV on day 1 and 200 mg IV on day 8 with optional third and fourth doses of 200 mg on day 15 and 22 if required. Treatment regimen in the caspofungin group was 70 mg IV on day 1 followed by 50 mg IV once daily for a minimum of 3 days and a maximum of 28 days. The primary endpoints were global cure at day 14 and 30-day all-cause mortality with an non-inferiority margin of 20% for both.
A total of 199 patients were randomized to either rezafungin (n = 100) or caspofungin (n = 99). The average age was 61 years and 81 (41%) were women. Global cure was achieved in 59% of the rezafungin group and 61% of the caspofungin group. A least one treatment-emergent adverse event was seen in 91% of the rezafungin group and 85% of the caspofungin group. 30-day all-cause mortality was 24% in the rezafungin group and 21% in the caspofungin group. Serious adverse events occurred in 56% of the rezafungin group and 53% of the caspofungin group. The most common treatment-emergent events were pyrexia, hypokalemia, pneumonia, septic shock, and anemia.
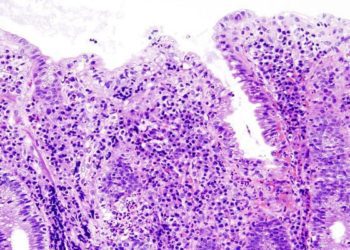
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.