Risankizumab induction therapy is effective for moderate-to-severe Crohn’s disease
1. The risankizumab group showed greater clinical remission and endoscopic response rates compared to placebo across the ADVANCE and MOTIVATE trials.
2. Treatment-related adverse events were mild and comparable between the three groups.
Evidence Rating Level: 1 (Excellent)
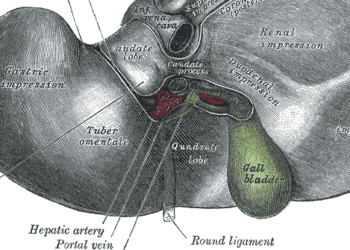
Study Rundown: Biologics are currently used as the first-line therapy for treatment of moderate-severe Crohn’s disease. However, a significant proportion of patients do not achieve adequate remission or have high rates of relapse despite biologics. It is believed that Risankizumab, an interleukin (IL)-23 inhibitor used to treat plaque psoriasis and psoriatic arthritis, may have a role in the treatment of active Crohn’s disease. However, current research in this regard is limited. This randomized controlled trial aimed to assess the safety and efficacy of risankizumab in patients with moderate-to-severe Crohn’s disease. Co-primary outcomes included clinical remission, as per the Crohn’s disease activity index (CDAI), and endoscopic response at 12 weeks from baseline. Key secondary outcomes included CDAI clinical response at weeks 4 and 12, as well as treatment-related adverse events. According to study results, risankizumab showed a greater clinical remission, compared to the controlled group, at various doses across the ADVANCE and MOTIVATE trials. Meanwhile, there were no significant differences in adverse events between the risankizumab and placebo groups. A major strength of this study is that it reported results from two simultaneous trials with a large sample size of patients from various centers, thus adding to the generalizability of the study.
Click to read the study in The Lancet
Relevant Reading: Risankizumab versus Ustekinumab for Moderate-to-Severe Plaque Psoriasis
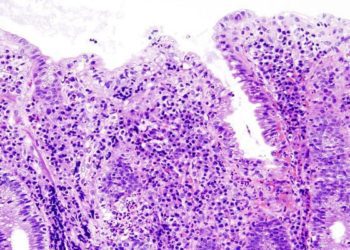
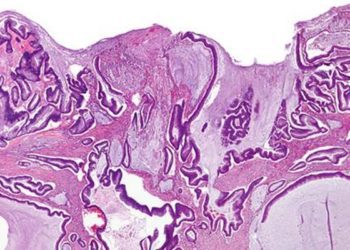
In-depth [randomized-controlled trial]: Between May 10, 2017, and Aug 24, 2020 (ADVANCE trial), and Dec 18, 2017, and Sept 9, 2020 (MOTIVATE trial), 1578 patients and 988 patients were assessed for eligibility in 40 countries. Included were those between 16-80 years old with moderate-to-severe Crohn’s disease and resistance to one or more biologics. Altogether, 797 patients in the ADVANCE trial (320 in risankizumab 600 mg, 327 in risankizumab 1200 mg, and 150 in placebo) and 530 patients in the MOTIVATE trial (185 in risankizumab 600 mg, 184 in risankizumab 1200 mg, and 161 in placebo) were included. The primary outcome of CDAI clinical remission was greater in the intervention group compared to controlled, across both trials (ADVANCE: 45% with risankizumab 600 mg, 42% with risankizumab 1200 mg, 25% with placebo, p<0.0001; MOTIVATE: 42% with risankizumab 600 mg; 40% with risankizumab 1200 mg; 20% with placebo, p<0.0001). Similarly, this was the case for endoscopic response (ADVANCE: 40% with risankizumab 600 mg; 32% with risankizumab 1200 mg; 12% with placebo vs. MOTIVATE: 29% with risankizumab 600 mg; 34% with risankizumab 1200 mg; 11% with placebo). Majority of treatment-related adverse events were mild with one treatment-independent death in the risankizumab group. Overall, findings from this study suggest that risankizumab may be used as induction therapy in patients with Crohn’s disease.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.