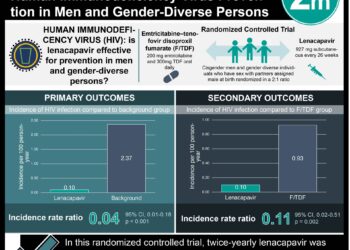
Risk scores perform moderately well in discriminating people living with HIV with higher vs lower cardiovascular disease risk
1. In this systematic review and meta-analysis, among the ten risk prediction scores analyzed, most risk scores had a moderate performance in discrimination, without a significant difference in performance between risk scores of the general and HIV-specific populations.
2. The Data Collection on Adverse Effects of Anti-HIV Drugs Cohort (D:A:D) 2016 model, Framingham Risk Score (FRS), and Pooled Cohort Equation (PCE) 10-year risk models had the highest performance in discrimination compared to the other risk scores analyzed.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Recent advancements in antiretroviral therapy have increased the lifespan of people living with HIV. With this, there is an increasing prevalence of noncommunicable diseases, in particular, cardiovascular disease (CVD), including myocardial infarction (MI) and stroke. Primary prevention measures such as the use of CVD risk-prediction tools can assist in identifying and targeting therapy for individuals living with HIV, who are at a higher risk for developing CVD. However, data on the performance of CVD risk score models in people living with HIV have not been synthesized. Hence, the objective of this study was to synthesize available data on the performance of the various CVD risk scores in people living with HIV. A total of nine observational studies were included in this review, involving 75 304 individuals living with HIV. From the included studies, 10 unique risk prediction models were compared in their ability to predict CVD risk in people living with HIV (6 in the general population and 4 in the HIV-specific population). The D:A:D 2016 model, FRS, and PCE model performed better in comparison to the other risk models evaluated. All models tended to underpredict CVD risk by 20% to 50%, with the exception of the FRS and PCE 10-year models, which were better calibrated. Risk models were found to perform moderately well in discriminating people living with HIV with a higher vs lower CVD risk, with a general tendency to underpredict. While a strength of this study is its large sample size, data was limited on comparative performance between different models and reclassification ability.
Click to read the study in JAMA Cardiology
Click to read an accompanying editorial in JAMA Cardiology
Relevant Reading: Cardiovascular risk prediction functions underestimate risk in HIV infection
In-Depth [systematic review and meta-analysis]: This study synthesized the available data on the performance of various CVD risk scores in people living with HIV. PubMed and Embase databases were searched from inception to January 2021. Included criteria for studies included cohort design, adults living with a diagnosis of HIV, CVD outcomes, and those that had available data on a minimum of 1 CVD risk score. The main measures were those of calibration and discrimination. A total of nine observational studies were included, involving a total of 75 304 (weighted average age, 42 years; 59 490 males [79%]) individuals living with HIV. A total of ten risk prediction scores were analyzed (6 in the general population and 4 in the HIV-specific population). Those that assessed the general population included FRS, PCE, Systematic Coronary Risk Evaluation (SCORE), the Cuore Project (CUORE), Framingham-Registre Gironi del COR (REGICOR), and Copenhagen risk score. Risk scores that were HIV-specific CVD risk prediction models included D:A:D 2010 model, D:A:D 2016 model, HIV Myocardial Infarction (HIVMI) score, and the Veterans Aging Cohort Study (VACS) Index. A majority of the risk scores analyzed demonstrated moderate performance in discrimination (C statistic: 0.7-0.8), without a significant difference in performance between the risk scores of the general and HIV-specific populations. The D:A:D model, FRS, and PCE 10 year, had the highest performance in discrimination.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.