Rivaroxaban does not prevent cardiovascular events in rheumatic heart disease patients with atrial fibrillation
1. Rivaroxaban was not associated with a lower rate of cardiovascular events and death compared to vitamin K antagonist treatment in patients with rheumatic heart disease-associated atrial fibrillation.
2. There was no significant differences between groups in the incidence of major bleeding safety outcomes.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Previous randomized trials have demonstrated the efficacy of non-vitamin K antagonist oral coagulants, such as the factor Xa inhibitor rivaroxaban, for stroke prevention in patients with atrial fibrillation. Compared to vitamin K antagonist treatment, Rivaroxaban treatment does not require regular blood sampling to monitor anticoagulation status. However, these trials have largely excluded patients with rheumatic heart disease. This randomized control trial evaluated the efficacy and safety of rivaroxaban for preventing cardiovascular events in patients with rheumatic heart disease-associated atrial fibrillation. Patients were followed for an average of 3.1 years. The incidence of a primary outcome event, defined as a composite of stroke, systemic embolism, myocardial infarction, or death, was higher in the rivaroxaban compared to the vitamin K antagonist group. Mortality was higher in the rivaroxaban group, owing to higher rates of sudden cardiac death or mechanical or pump failure. Rates of hospitalization for heart failure and valvular replacement surgery were not significantly different between groups. There were no significant differences in rates of major bleeding, the primary safety outcome, between groups. As a limitation, there was a higher incidence of discontinuation of rivaroxaban than vitamin K antagonist, which may lead to more cardiovascular events in the rivaroxaban group. In addition, outcome measures had to be redefined during the trial due to lower rates of cardiovascular events than expected.
Click to read the study in NEJM
In-Depth [randomized controlled trial]: In the present randomized control trial, adults aged 18 and over with documented atrial fibrillation and echocardiographically-confirmed rheumatic heart disease (n=4,531) were recruited at 138 trial sites in Africa, Asia, and Latin America. Patients were randomly assigned in a 1:1 ratio to receive either rivaroxaban (n=2,275) or a locally available vitamin K antagonist (n=2256). According to renal function, Rivaroxaban was administered at a daily dose of 15 or 20mg. The most administered vitamin K antagonist was warfarin (79 to 85% of patients in the group). Patients were followed for up to one month after randomization and every six months afterward for a mean follow-up of 3.1 (standard deviation, 1.2) years. The incidence of trial discontinuation was higher in the rivaroxaban group compared to the vitamin K antagonist group (79.0% and 96.4% adherence respectively at year four). A primary-outcome event, defined as stroke, systemic embolism, myocardial infarction, or death, occurred in 560 and 446 patients in the rivaroxaban and vitamin K antagonist groups, respectively (proportional-hazards ratio, 1.25; 95% Confidence Interval [CI], 1.10 to 1.41). For secondary outcomes, both incidences of stroke (90 and 65 patients in the rivaroxaban and vitamin K antagonist groups, respectively) and mortality (difference in restricted mean survival time, -72 days; 95% CI, -117 to -28) were higher in the rivaroxaban group. Rates of hospitalization for heart failure or valvular replacement surgery were not significantly different between groups. There were no significant differences in rates of major bleeding. Results from this trial support current guidelines that recommend vitamin K antagonists, and not rivaroxaban, for stroke prevention in patients with rheumatic heart disease-associated atrial fibrillation.
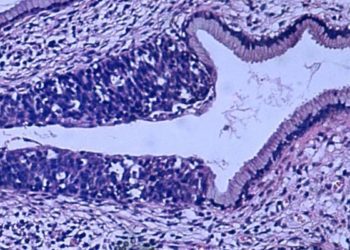
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.




![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-75x75.jpg)

