Screening insufficient for newborns exposed to hepatitis C virus
1. In this retrospective study, only a fraction of infants receiving well-child care at the study institution were screened for hepatitis C, despite being born to mothers with a known history of hepatitis C virus infection.
2. Opioid use in mothers was the only factor positively associated with practitioners accurately identifying the need for hepatitis C virus testing.
Evidence Rating Level: 2 (Good)
Study Rundown: In the context of the widespread opioid epidemic, Hepatitis C viral (HCV) infection rates have increased in recent years. With this rise comes the additional risk of transmission from mother to child during childbirth, with perinatal transmission being the leading cause of infection in children. All children born to mothers with HCV infection should undergo viral screening, but few are properly tested at 18 months of age or older, in-line with national guidelines. Researchers at the University of Pittsburgh performed a review of pregnant women infected with HCV who both delivered their children and whose children subsequently received care at their institution. Of this group, only 30% of children were properly screened for HCV. Moreover, only opioid use disorder specifically was associated with practitioners positively identifying the need for HCV virus testing. Despite this study’s limitations by potential use of inaccurate ICD-9 codes as a source of data, the results demonstrate the need to make HCV testing more standardized for those children born to women infected with HCV.
Click here to read the original article, published today in Pediatrics
Relevant Reading: Vertical Transmission of Hepatitis C Virus: Systematic Review and Meta-analysis
In-Depth [retrospective cohort]: Researchers retrospectively reviewed whether or not pregnant women with known HCV had their children subsequently screened in an appropriate and timely manner. The study population received care at Magee-Women’s Hospital at the University of Pittsburgh, a large tertiary care facility where many women were anticipated to both deliver and subsequently receive well-child care. Data was drawn from January 1, 2006 to December 31, 2014. Of the 87 924 women who delivered during this time period, only 1043 (1.2%) were identified as having HCV and thus eligible for the study. Over the study’s nine-year time period, the incidence of HCV infection in mothers increased 60%. Of the 1043 infants delivered to mothers with HCV, 323 (32%) had a hemoglobin or lead level documented in the chart, indicating they were receiving well-child care at the University of Pittsburgh. Of those receiving well-child care, only 96 (30%) were screened in some fashion for HCV. Of the 96 children screened, 73 (76%) had an optimal initial screen. The remaining 23 children had suboptimal screening for a variety of reasons, including 11 (48%) children in whom HCV antibody tests were sent before 18 months of age and 12 (52%) children in whom HCV PCR tests were sent after 18 months of age. Only maternal opioid use disorder—as opposed to tobacco use or other substance use—was positively associated with an increase in the accurate identification of the need for HCV testing in the child (p=.02).
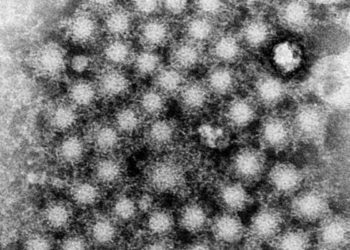
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.