Sepsis performance measure implementation not associated with clinical outcomes improvement
1. Adoption of the Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) program resulted in greater adherence to individual process measures such as lactate measurement, early antibiotics, and fluid therapy.
2. These increases were variable in magnitude and did not associate with meaningful changes in sepsis outcomes.
Evidence Rating Level: 2 (Good)
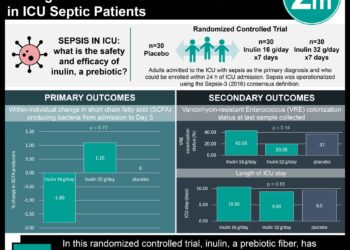
Study Rundown: Sepsis is associated with significant mortality and consistently ranks among the costliest inpatient conditions in the United States. Evidence-based protocols for early sepsis therapy have been shown to reduce preventable morbidity and mortality, but there has been pushback against mandatory adherence due to clinician concerns regarding unintended harms, including antimicrobial resistance and unnecessary diversion of health care resources. As such, this study evaluated the longitudinal changes in sepsis treatment and outcomes that arose from SEP-1 implementation. SEP-1 implementation was associated with substantial increases in three-hour lactate measurement and six-hour repeat lactate measurement as well as minor increases in antibiotic administration and intravenous fluid administration. However, statistically significant between-group differences were not observed in any of the three clinical outcomes of intensive care unit admission, in-hospital mortality, or home discharge. This study was limited by the lack of a control group and thus relied on the assumption that sepsis trends were unchanged over the study period. Overall, these results suggested that SEP-1 had variable effects on target clinical outcome measures for sepsis.
Click here to read the study in Annals of Internal Medicine
Relevant Reading: Evidence underpinning the Centers for Medicare & Medicaid Services’ Severe Sepsis and Septic Shock Management Bundle (SEP-1): a systematic review.
In-Depth [retrospective cohort]: This longitudinal study utilized electronic health record data from 11 hospitals in the University of Pittsburgh Medical Center (UPMC) Health System from January 2013 to December 2017. The study encompassed 54,255 unique patient encounters. Patients who met the criteria of suspected infection and organ dysfunction within six hours of arrival to the emergency department (ED) were included in the study. Patients excluded from the study were those transferred to the ED and repeated encounters. SEP-1 implementation led to dramatic increases in adherence to three-hour lactate measurement (absolute difference, 23.7 percentage points; 95% confidence interval [CI], 20.7 to 26.7 percentage points; P < 0.001) and six-hour repeat lactate measurement (absolute difference, 17.4 percentage points; 95% CI, 14.4 to 20.4 percentage points; P < 0.001). Clinical outcomes were generally similar in the pre-SEP-1 and post-SEP-1 periods; ICU admissions were numerically greater (absolute difference, 2.0 percentage points; 95% CI, 0 to 4.0 percentage points; P = 0.055), as was mortality (absolute change, 0.1 percentage points; 95% CI, -0.9 to 1.1 percentage points; P = 0.87). Consequently, fewer patients were discharged home (absolute difference, -1.8 percentage points; 95% CI, -4.1 to 0.6 percentage points; P = 0.145). Overall, SEP-1 implementation was not shown to result in a meaningful association with changes in sepsis outcomes.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.