Sequencing of androgen-deprivation therapy with radiotherapy for non-metastatic prostate cancer
1. Concurrent/adjuvant androgen-deprivation therapy has improved metastatic-free survival compared to neoadjuvant/concurrent androgen-deprivation therapy.
2. The statistical significance was mainly seen in patients who had prostate-only radiation, and not seen in patients who had whole-pelvis radiation.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Androgen-deprivation therapy (ADT) when added to radiotherapy (RT) has been shown to improve survival for localized prostate cancer, but the optimal sequencing of ADT has not been determined. This study contains pooled data from 12 randomized trials to examine whether neoadjuvant/concurrent or concurrent/adjuvant ADT leads to better outcomes. The primary endpoints were metastatic-free survival (MFS), and secondary endpoints included overall survival (OS), biochemical recurrence (BCR), distant metastasis (DM), prostate cancer specific mortality (PCSM), and other-cause mortality. Not all patient characteristics were equal in both groups as it was found that the concurrent/adjuvant ADT group had higher levels of high-risk disease than in the neoadjuvant/concurrent ADT group. The study also analyzed subgroups of RT and found that there were differences in patients who received prostate-only RT (PORT) and those who received whole-pelvis RT (WPRT). This study found that in the whole population, the concurrent/adjuvant ADT group had improved MFS (64.9% vs 61.4% in 10-year estimate), BCR (27.5% vs 33.7%), PCSM (6.5% vs 7.7%), and OS (68.8% vs 64.7%) than patients in the neoadjuvant/concurrent ADT group, but the statistical significance was only seen in the PORT group. The strengths of this study include the large population size, the number of studies, and the subgroup analysis. Limitations of this study include a non-homogeneous baseline characteristic. Overall, this study suggests that concurrent/adjuvant ADT is the optimal sequence for prostate-only radiation.
Click to read the study in JCO
In-Depth [meta-analysis]: This study contains 7,409 patients from 12 randomized trails that enrolled patients receiving neoadjuvant/concurrent (started more than 2 months prior to RT) or concurrent/adjuvant (started with RT and used for more than 2 months after finishing RT) short term ADT (4-6 months) with RT. Analysis was conducted on an intention-to-treat basis. Median follow-up time was 10.2 years. Patients (1,084) in the concurrent/adjuvant ADT group a more often had high-risk disease than patients (6,325) in the neoadjuvant/concurrent ADT group. The study found that overall, patients in the concurrent/adjuvant ADT group had improved MFS than patients in the neoadjuvant/concurrent ADT group, with 10-year estimates of 64.9% v 61.4% (95%CI, 0.74 to 0.93), but this was mainly seen in patients receiving PORT who had a HR 0.65 (95%CI, 0.54 to 0.79), compared to those who had WPRT (HR 0.94, 95%CI, 0.79 to 1.12). Overall, concurrent/adjuvant ADT was also associated with improved BCR (27.5% vs 33.7%, 95% CI, 0.68 to 0.87), PCSM (6.5% vs 7.7%, 95% CI, 0.59 to 0.99), and OS (68.8% vs 64.7%, 95% CI, 0.70 to 0.89), but when further analyzed, the statistical significance was mostly seen in patient with PORT and not in patient with WPRT. There were no overall significant differences in DM observed (12.0% vs 10.2%, 95% CI, 0.95 to 1.39), but in patients with WPRT there was an associated increase in incidence of DM. Overall this study found that concurrent/adjuvant ADT is associated with better outcomes, but only in those patients who receive prostate-only radiation.
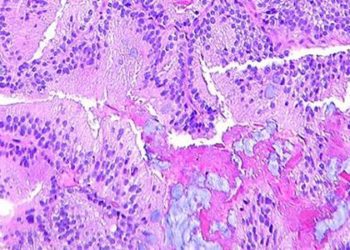
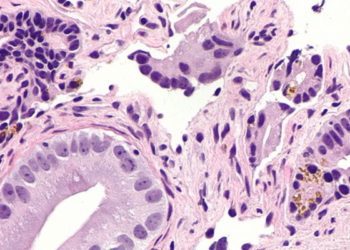
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.