Serum hCG equal to ultrasonography in medical abortion follow-up
Feb 16th – After medical abortion, both serum hCG and ultrasonography have low rates of unplanned intervention and are equally acceptable forms of follow-up.
[tabs tab1=”2MM Rundown” tab2= “2MM Full Report”]
[tab]
Image: PD
1. After medical abortion, both serum hCG and ultrasonography have low rates of unplanned intervention and are equally acceptable forms of follow-up.
2. Patient preference should be used to decide method of follow-up after abortion.
The present study is the first randomized controlled trial to compare follow-up after medical abortion via serum hCG versus the more traditional method of transvaginal ultrasound. Results found that both methods are acceptable forms of follow-up, evidenced by similarly low rates of unplanned interventions and similarly high rates of patient satisfaction. Given the unique pros and cons of each method (discomfort of needle stick vs. transvaginal ultrasound, drawback of requisite return clinic visits for ultrasound but benefit of visual confirmation) these findings suggest the method of surveillance can be based on patient preferences.
The study population was homogenous, mainly consisting of young (average age 26), white, English-speaking, single, educated women, and thus results may not be generalizable to other study groups. Another notable limitation is the study’s lack of long term follow-up. Specifically, hCG surveillance may result in unplanned interventions related to lack of visualization of the uterine cavity, which would not present themselves until more than four weeks after the procedure, outside the time period examined in this study. Further studies should be targeted at evaluating these methods in a more heterogeneous population with long-term follow-up.
Click to read the study in Obstetrics & Gynecology
Click to see the clinical trial registration
[/tab]
[tab]
Image: PD
1. Both serum hCG and ultrasonography have low rates of unplanned intervention and are equally acceptable forms of follow-up for medical abortions.
2. Patient preference should be used to decide method of follow-up.
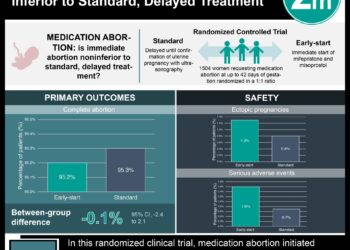
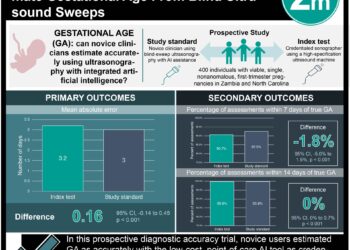
This [prospective randomized controlled] trial: randomized 376 women undergoing medical abortion to either the serum hCG (n=159) or transvaginal ultrasound (n=151) follow-up. The primary outcome was unplanned interventions measured as a composite combining additional clinic/emergency room visits, repeat dosing of misoprostol, and need for surgical evacuation. Secondary outcome was patient satisfaction with assigned method of follow-up. Outcome ascertainment was performed via follow-up surveys and confirmed by retrospective medical record review.
Within two weeks after medical abortion, 8.2% of women receiving hCG follow-up and 6.6% of women receiving ultrasonography follow-up experienced an unplanned intervention (CI: 0.56-2.73, p=0.6). At four weeks, 1.4% of women in the hCG arm versus 4.4% in the ultrasound arm met primary outcome (CI: 0.07-1.54, p=0.16). There was no significant difference in the type of unplanned intervention required. Overall, patients in both arms expressed satisfaction with their care (88% hCG vs 95% ultrasound, p=0.25).
In sum: The present study is the first randomized controlled trial to compare follow-up after medical abortion via serum hCG versus the more traditional method of transvaginal ultrasound. Results found that both methods are acceptable forms of follow-up, evidenced by similarly low rates of unplanned interventions and similarly high rates of patient satisfaction. Given the unique pros and cons of each method (discomfort of needle stick vs. transvaginal ultrasound, drawback of requisite return clinic visits for ultrasound but benefit of visual confirmation) these findings suggest the method of surveillance can be based on patient preferences.
The study population was homogenous, mainly consisting of young (average age 26), white, English-speaking, single, educated women, and thus results may not be generalizable to other study groups. Another notable limitation is the study’s lack of long term follow-up. Specifically, hCG surveillance may result in unplanned interventions related to lack of visualization of the uterine cavity, which would not present themselves until more than four weeks after the procedure, outside the time period examined in this study. Further studies should be targeted at evaluating these methods in a more heterogeneous population with long-term follow-up.
Click to read the study in Obstetrics & Gynecology
Click to see the clinical trial registration
By Maren Shapiro and Leah Hawkins
More from this author: New worldwide target for reducing preterm births by 2015, No cost contraception reduces unintended pregnancies, Active-Duty U.S. servicewomen have higher rates of unintended pregnancy
[/tab]
[/tabs]