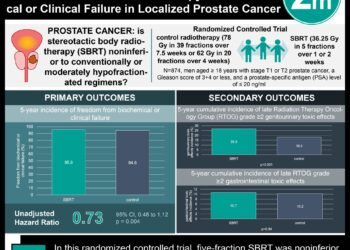
Similar prostate cancer mortality with surgery, radiation, and active surveillance: The ProtecT trial
1. The rate of prostate-cancer-specific mortality was nonsignificantly different for active surveillance, radical prostatectomy, and external beam radiation therapy over a median follow-up period of 10 years.
2. Rates of disease progression and metastases were significantly higher in the active surveillance group than in the treatment groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Clinical decision making for the management of prostate cancer has become increasingly complex in recent years as widespread PSA testing and expansion of active surveillance have become popularized. It is well known that many men with prostate cancer will go on to succumb to competing causes other than this disease, the ability to predict who these men are is limited.
In the Prostate Testing for Cancer and Treatment (ProtecT) trial, 1643 men with newly diagnosed prostate cancer were randomly assigned to active surveillance, radical prostatectomy, or 3D conformal, external beam radiotherapy (EBRT). The outcomes they measured for a median follow-up period of 10 years were prostate-cancer-related deaths, all-cause mortality, rates of metastases, clinical progression, primary treatment failure, and treatment complications.
A non-significant difference was observed for prostate-cancer-specific death was found between the three groups. A non-significant difference was observed for all-cause mortality between the three groups. The rate of disease progression and the rate of metastasis was significantly greater in the active surveillance groups than in the treatment groups. This study draws strength from its comparison of the effectiveness of the three major contemporary treatment modalities for prostate cancer among a large population for a long follow-up period of a median of 10 years. However, as the trial began in 1999 the generalizability of these results is limited by the lack of inclusion of therapeutic advances that were not in practice at that time such as robot-assisted prostatectomy, intensity modulated radiotherapy, and brachytherapy.
Click to read the study, published today in NEJM
Relevant Reading: Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer
In-Depth [randomized controlled trial]: This three-arm, prospective, randomized controlled trial randomized 1643 men with newly diagnosed localized prostate cancer to active surveillance (n = 545), radiation therapy (n = 545), and radical prostatectomy (n = 553) groups. There were 8 prostate-cancer-specific deaths in the active surveillance group (1.5 deaths per 1000 person-years; 95%CI 0.7 to 3.0), 5 prostate-cancer-specific deaths in the surgery group (0.9 per 1000 person-years; 95%CI 0.4 to 2.2), and 4 prostate-cancer-specific deaths in the radiotherapy group (0.7 per 1000 person-years; 95%CI, 0.3 to 2.0) (p = 0.48 for the overall comparison). There was no significant difference in all-cause mortality between the 169 deaths within the three groups (p = 0.87, for the comparison along the three groups). A total of 33 men developed metastases in the active surveillance group, 13 men developed metastases in the prostatectomy group, and 16 men developed metastases in the radiotherapy group (p = 0.004, for overall comparison). 112 men demonstrated disease progression in the active surveillance group, 46 men demonstrated disease progression in the prostatectomy group, and 46 men demonstrated disease progression in the radiotherapy group (p < 0.001 for the overall comparison).
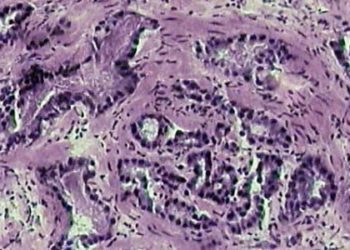
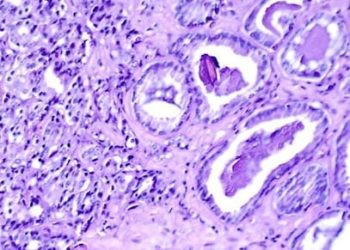
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.