Small-molecule inhibitor may reduce chemotherapy-associated metastases [PreClinical]
1. In a mouse model of breast cancer, treatment with the chemotherapy paclitaxel (Ptx) enhanced tumor cell dissemination and the formation of micrometastatic lung lesions.
2. Prophylactic treatment with rebastinib diminished Ptx-driven metastatic progression by reducing levels of circulating tumor cells (CTCs) in the blood.
Evidence Rating Level: 2 (Good)
Study Rundown: Though chemotherapeutic agents are widely used as neoadjuvant therapies for treating a variety of cancers including breast cancer, increasing scientific evidence suggests that these drugs may in fact result in disease progression. In this work, the authors demonstrated that Ptx treatment enhanced the metastasis of breast cancer, then investigated the efficacy of a secondary treatment to mitigate this effect.
Using mice with spontaneous or transplanted breast tumors, the authors demonstrated that treatment with Ptx diminished tumor volume. However, treatment also enhanced metastatic dissemination, as measured by the number of hematogenous CTCs, and resulted in a higher rate of lung metastasis. This effect was accompanied by a higher tumor microenvironment of metastasis (TMEM) score, which quantifies the microanatomical sites that are known to be associated with hematogenous entry of cancer cells and serves as clinical marker of metastasis in breast cancer patients. When mice received pretreatment with rebastinib, a known inhibitor of the TIE2 receptor that is expressed by TMEM-associated macrophages, TMEM scores did not significantly change. Nonetheless, this combination therapy diminished overall CTC levels.
While this work provides preliminary evidence that treatment with rebastinib during chemotherapy can diminish CTC levels, future work should focus on directly demonstrating lower incidence of metastasis and improved overall survival. Additionally, safety studies will need to determine proper dosage and treatment regimen to maximize efficacy while minimizing off-target effects.
Click to read the study in Science Translational Medicine
Relevant Reading: Tumor Microenvironment of Metastasis in Human Breast Carcinoma: A Potential Prognostic Marker Linked to Hematogenous Dissemination
In-Depth [animal study]: Two mouse models of breast cancer were established for these experiments: (1) spontaneous breast tumors developed in FVB transgenic mice expressing the Polyoma Virus Middle-T (PyMT) antigen under the control of mammary tumor virus long terminal repeat (MMTV-LTR), and (2) late-stage carcinomas from spontaneous PyMT tumors were transplanted into 5–6 week old recipient FVB mice. Both groups received Ptx intravenously at 10 mg/mL every 5 days for a total of 3 doses.
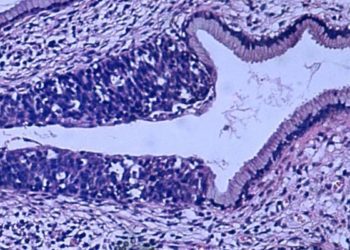
As compared to vehicle control treatment, Ptx-treated mice demonstrated a minor decrease in tumor volume (p = 0.08) and nearly two-fold increases in TMEM score (p < 0.001), as measured by colocalization of MENA, IBA1, and endomucin via immunohistological staining. Levels of CTCs were measured prior to sacrifice on day 15, and results indicated an increase in CTCs after Ptx treatment relative to the control (p < 0.005). Quantifications of disseminated single cells and micrometastatic foci (clusters with >5 cancer cells) were determined through H&E staining. Ptx treatment resulted in nearly twice as many disseminated single cells (p = 0.008) and increased incidence and number of lung metastases.
To determine the effects of rebastinib on Ptx-induced metastatic progression, mice were treated daily through oral administration of 10 mg/kg rebastinib for 4 days prior to Ptx administration and throughout the chemotherapy regimen. Though TMEM scores did not significantly differ between the Ptx-only and Ptx+rebastinib groups, the combination treatment significantly lowered CTC levels in the blood (p = 0.0012).
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.