Small molecule inhibitor may resolve parasitic infections of neglected tropical diseases [PreClinical]
1. In several mouse models, a novel small molecule inhibitor, GNF6702 (GNF), effectively cleared infections of parasites that cause leishmaniasis, Chagas disease (CD), and human African trypanosomiasis (HAT).
2. GNF inhibited the activity of the parasite proteasome and showed little off-target effects on the human proteasome when tested in vitro.
Evidence Rating Level: 2 (Good)
Study Rundown: Leishmaniasis, CD, and HAT are parasitic diseases caused by the parasites Leishmania, Trypanosoma (T.) cruzi, and T. brucei, respectively. Though these illnesses affect 20 million people worldwide, treatments are limited in efficacy and availability, especially in underdeveloped regions where these diseases are most prevalent. In this work, researchers identified a drug that effectively cleared parasitic infections with promise to minimize off-target effects.
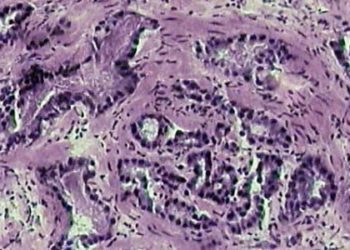
In mice with two forms of leishmaniasis, treatment with GNF led to a significantly greater reduction in parasite burden as compared to treatment with miltefosine, the only oral anti-leishmaniasis therapy clinically available. To test drug efficacy against T. cruzi, infected mice were treated with GNF or benznidazole, a commonly used treatment that often causes severe side effects and treatment discontinuation. The efficacy of GNF treatment was comparable to that of benznidazole treatment, where all but one animal had undetectable levels of parasite in the blood, colon, and heart tissue. Finally, GNF was tested in mice with T. brucei infection. Results indicated that GNF retained clearance of parasites in the brain of diseased mice whereas treatment with diminazine aceturate, a clinically used treatment, resulted in reestablishment of T. brucei infection over time. Through various in vitro techniques, researchers determined that GNF minimizes parasite burden by the parasite proteasome common between all three strains of kinetoplastid parasites. Using a broad-spectrum screening tool, GNF was found to not significantly affect the activity of various human enzymes and receptors when compared to the vehicle control.
This work provides promising new insights into a molecular target for kinetoplastid parasite diseases and a potential new therapeutic agent, but more focused research to validate safety and long-term efficacy in animal models will need to continue before entering clinical trials.
Click to read the study in Nature
Relevant Reading: The Kinetoplastid Chemotherapy Revisited: Current Drugs, Recent Advances and Future Perspectives
In-Depth [animal study]: To model leishmaniasis, female BALB/c mice were infected with Leishmania donovani (visceral form) or Leishmania major (cutaneous form) through tail vein injection and injection into the hind footpad, respectively. Eight-day treatment with GNF (10mg/kg) in the visceral group (n=5) resulted in a three-log reduction of parasite burden in the liver when compared to treatment with miltefosine. In the cutaneous form (n=6), twice-daily treatment with 10mg/kg GNF resulted in a five-fold reduction in footpad parasite burden when compared to miltefosine treatment (30mg/kg once-daily). In the model for CD, female C57BL/6 mice were intraperitoneally injected with T. cruzi trypomastigotes. Thirty-five days after infection, the mice received daily doses of 100mg/kg benznidazole or twice-daily doses of 10mg/kg GNF. After 20 days of treatment, samples were collected from the brain, heart, and colon. The GNF-treated group performed similarly to the control group. Finally, HAT was modeled through peritoneum injection of T. brucei. After 21 days of infection, treatment was administered for 7 days as either oral lavage of 100mg/kg GNF or intraperitoneal injection of 40mg/kg diminazine aceturate. In vivo bioluminescence was used to quantify parasite burden 28, 42, and 92 days after infection. Whereas mice treated with GNF exhibited little to no bioluminescence throughout the body and the brain, the diminazine aceturate group experience reestablishment of infection as early as 42 days after infection.
Using in vitro techniques to generate mutations in the PSMB4 proteasome protein, GNF was found to be a selective inhibitor of the parasitic proteasome. Lastly, by using a broad panel of molecular assays, GNF (10uM) was predicted to have little effect on the human proteasome.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.