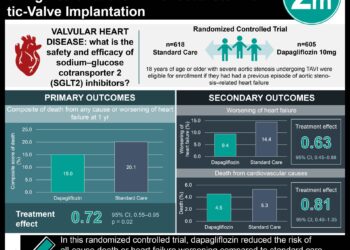
Sotagliflozin reduces cardiovascular risk for patients with diabetes and worsening heart failure
1. Sotagliflozin was shown to lower the risk of total number of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure in patients with diabetes and recent worsening heart failure compared to placebo.
2. Sotagliflozin was shown to be similar in the percentage of patients with adverse events leading to study withdrawal compared to the placebo.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Sodium-glucose cotransporter 2 (SGLT2) inhibitors lower hospitalization risk for heart failure in patients with type 2 diabetes. Furthermore, SGLT2 inhibitors reduce risk of death from cardiovascular causes. However, safety concerns have arisen with SGLT2 inhibitor treatment such as hypotension risk and precipitation of kidney failure. Additionally, the efficacy of SGLT2 inhibitors for patients with heart failure remains unknown. As such, this study determined the safety and efficacy of starting sotagliflozin, a SGLT1/2 inhibitor, treatment after an episode of decompensated heart failure in patients co-diagnosed with type 2 diabetes. The study reported sotagliflozin treatment reduced the risk of death from cardiovascular causes, hospitalization for heart failure, and urgent visits for heart failure. The randomized control trial was limited by the loss of funding prior the completion of participant enrollment of the initial planned sample size. Therefore, the assessment of endpoints such as death from cardiovascular causes was limited. Nonetheless, this study’s results are significant, and its findings highlight the effectiveness of sotagliflozin treatment in reducing adverse cardiovascular risk in patients with type 2 diabetes and recent worsening heart failure.
Click to read the study in NEJM
Relevant Reading: Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure
In-Depth [randomized controlled trial]: This randomized control trial enrolled 1,222 participants in a multicenter study at 306 sites in 32 countries. Participants included in the study were between 18 and 85 years of age with a previous type 2 diabetes diagnosis, hospitalized with signs and symptoms of heart failure, and received intravenous diuretic treatment. Participants with end-stage heart failure, recent percutaneous or coronary artery bypass graft intervention, and an estimated glomerular filtration rate (eGFR) of less than 30 mL per minute per 1.73cm2 were excluded from this study. The participants were randomized in a 1:1 ratio to receive once daily, 200 mg of sotagliflozin or placebo, respectively. The primary endpoint was the total number of deaths from cardiovascular causes, hospitalization for heart failure, and urgent visits for heart failure. During the study, a total of 600 primary endpoints occurred among the participants (245 in the sotagliflozin group and 355 in the placebo group). The rate of total primary endpoint was 51.0 events per 100 patient-years in the sotagliflozin group compared to 76.3 events per 100 patient-years in the placebo (hazard ratio, 0.67; 95% confidence interval [CI], 0.52 to 0.85; P<0.001). The absolute difference between the two group was 25.3 events per 100 patient-years (95% CI, 5.1 to 45.6). Specifically, the total number of hospitalizations for heart failure and urgent visits for heart failure was 40.4 events per 100 patient-years in the sotagliflozin group compared to 63.9 events per 100 person-years in the placebo (hazard ratio, 0.64; 95% CI, 0.49 to 0.83; P<0.001). Additionally, there was no significant difference between sotagliflozin (10.6 events per 100 patient-years) and placebo (12.5 events per 100 patient-years) in deaths from cardiovascular causes (hazard ratio, 0.84; 95%CI, 0.58 to 1.22; P<0.36). Finally, there was no statistical difference for the percentage of participants with adverse events leading to withdrawal between the two groups. The percentage of participants with serious adverse events was 3.0% in the sotagliflozin group compared to 2.8% in the control group. Certain events were more common in the sotagliflozin group compared to the control such as hypotension (6.0% vs. 4.6%) and diarrhea (6.1% vs. 3.4%). Taken together, sotagliflozin significantly lowered the risk of adverse cardiovascular events in participants with type 2 diabetes and acute decompensated heart failure.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.