Spinal anesthesia not superior to general anesthesia for hip surgery
1. Spinal anesthesia was not superior to general anesthesia for hip surgery in older adults in survival and ambulatory status at 60 days.
2. Postoperative delirium rate was similar between the spinal and general anesthesia groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Surgery is the standard of care for hip fractures, using either spinal or general anesthesia. While some observational evidence suggested that spinal anesthesia might offer better recovery and fewer complications, randomized trials are inconclusive and outdated from current practice. Especially, there is a lack of trials investigating the recovery of walking ability after the procedure, an important outcome for patients. The current study aimed to evaluate the recovery of ambulation of older adults following hip surgery utilizing spinal anesthesia, compared to general anesthesia. The primary outcome was a composite of death or an inability to walk 10ft independently at 60 days after randomization, it was shown that the primary outcome was comparable between the two patient groups. Similarly, the rates of death and delirium at 60 days and hospital length of stay were not different between the two anesthesia regimens. Notable limitations include missing outcome data and heterogeneity in sedation techniques. Nonetheless, the trial showed that in older patients undergoing hip surgery, spinal anesthesia was not superior to general anesthesia in risk of death or inability to walk independently at 60 days.
Click here to read the study in NEJM
Relevant Reading: General versus regional anaesthesia for hip fractures. A pilot randomised controlled trial of 322 patients
In-Depth [randomized controlled trial]: This pragmatic randomized trial enrolled 1600 patients 50 years of age or older who were undergoing surgical repair of hip fractures at 46 U.S. and Canadian centers. Patients were included based on age and diagnosis of femoral neck, intertrochanteric or subtrochanteric hip fracture. Patients were excluded if they had not been able to walk 10ft independently prior to the fracture, if the fracture was periprosthetic, if they were at risk of malignant hyperthermia, or if spinal anesthesia was contraindicated. Patients were randomized 1:1 to receive spinal anesthesia (by a single-injection spinal anesthetic coupled with appropriate sedation) or general anesthesia (with an inhaled maintenance anesthetic). Crossover between the anesthetic regiments occurred in 15% of patients assigned to spinal anesthesia and 3.5% of those assigned to general anesthesia. Modified intention-to-treat analysis included 1599 patients. The primary outcome was a composite of death and an inability to walk 10ft independently at 60 days after randomization. Secondary outcomes included the rates of death, new inability to walk at 60 days in alive patients, new-onset delirium, and length of hospital stay. The mean age of the patient population was 78% and 67.0% were women. In the modified intention-to-treat population, the composite primary outcome occurred in 18.5% patients undergoing spinal anesthesia and 18.0% in those undergoing general anesthesia (relative risk [RR], 1.03; 95% confidence interval [CI], 0.84 to 1.27; P=0.83). Within this composite outcome, death occurred in 3.9% of patients in the spinal anesthesia group and 4.1% in the general anesthesia group (RR, 0.97; 95% CI, 0.59 to 1.57), while an inability to walk independently was reported in 15.2% and 14.4%, respectively (RR, 1.06; 95% CI, 0.82 to 1.36). Furthermore, new-onset delirium occurred in 20.5% of patients in the spinal anesthesia group and 19.7% in the general anesthesia group (RR, 1.04; 95% CI, 0.84 to 1.30). The median length of hospital stay was identical between the two groups: 6 days for Canadian centers (hazard ratio [HR], 0.92; 95% CI, 0.76 to 1.10) and 3 days for U.S. centers (HR, 1.06; 95% CI, 0.96 to 1.16). The incidence of other adverse events was similar between the two regimens. The trial was significant in its focus on the recovery of the ability to walk as a primary outcome following hip fracture surgery, as well as examining outcomes beyond hospital discharge. Despite limitations regarding missing data and variability of sedation protocol during spinal anesthesia, the study showed that spinal anesthesia was not superior to general anesthesia for hip fracture surgery in older adults.
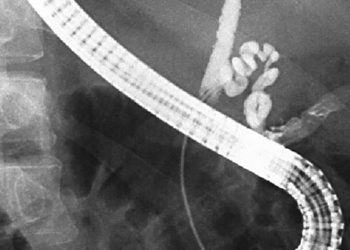
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.