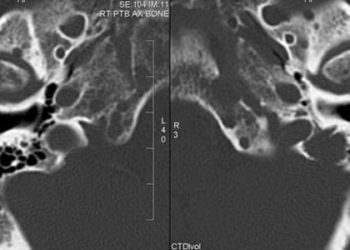
Stereotactic radiosurgery promising for patients with multiple brain metastases
Image: PD
1. In terms of overall survival, stereotactic radiosurgery for patients with five to ten brain metastases was non-inferior to same treatment for those with two to four metastases.
2. Radiation-related adverse neurological events were similar in both comparison groups.
Evidence rating: 2 (Good)
Study Rundown: Whole brain radiation therapy (WBRT) is a widely employed palliative treatment for brain metastases that is associated with severe toxicity to neurological function. It was previously demonstrated that stereotactic radiosurgery is similarly effective as WBRT in treating up to four metastatic lesions, with much less neurological toxicity. In this prospective observational study, the authors showed that patients with five to ten brain metastases treated only with radiosurgery fared equally well both in terms of overall survival and adverse neurological effects as compared to those treated for two to four lesions. The implicit extension of this study was that stereotactic radiosurgery would be equally effective for this multitude of brain metastases as compared to conventional WBRT. A limitation of this study was that higher-resolution MRI was not used, which may have underestimated the number of metastases in each comparison group. While the proportions of different primary cancers were balanced in each group, this was not done on a histopathological basis, which may have ignored finer subclass effects. Finally, while the results are inherently limited by the study design lacking randomization to WBRT, it does establish a foundation for such a study, which is currently being undertaken.
Click to read the study in Lancet Oncology
Click to read commentary in Lancet Oncology
Relevant reading: Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial
In Depth [prospective, observational study]: In this prospective, observational study, 1194 patients with brain metastases were selected for treatment with stereotactic radiosurgery. The participants were divided into three groups: those with one brain metastasis (n=455), those with two to four (n=531), and those with five to ten (n=208). The groups were matched in terms of age, sex, primary cancer, baseline neurological function, and tumor size. The median follow-up time after stereotactic surgery was 20.9 months. Median overall survival for patients with five to ten lesions was 10.8 months as compared to 10.8 months for those with two to four lesions (Hazard ratio 0.97, 95% confidence interval 0.8-1.18, p=0.78). This trend in non-inferiority was true regardless of primary cancer including lung, breast, GI, and kidney. Deterioration in neurological function at 24 months follow-up was seen in 13% of patients with five to ten lesions as compared to 11.6% of those with two to four lesions (HR 1.15, 95% CI 0.76-2.85, p=0.54). Outcomes were analyzed with intention-to-treat. Fischer’s exact test, student t-test, or Wilcoxon rank sum test were used to assess significance of comparisons.
More from this author: Erlotinib does not demonstrate increased survival in ovarian epithelial carcinomas, Afatinib shows increased progression-free survival in non-small-cell lung cancer, Slight increased risk of intussusception linked to rotavirus vaccination, Escalated-dose radiotherapy did not increase survival in prostate cancer
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.