Study site selection in trials pertaining to transcatheter valvular therapies can affect the socioeconomic makeup of the sample
1. Amongst hospitals with a cardiac surgery department, 11.5% participated actively in research trials of transcatheter mitral or tricuspid therapies.
2. Trial sites tended to serve a smaller proportion of socioeconomically disadvantaged individuals than did non-trial sites, but the ethnic makeup of patients was not different between the hospitals.
Level of Evidence Rating: 2 (Good)
Study Rundown: Trial selection in the past has been known to exclude certain groups, notably ethnic minorities, individuals of low socioeconomic status, and women. This creates uncertainty regarding the ability to apply evidence-based medicine to the treatment of all patients and thus can lead to inequities in healthcare. This study sought to describe demographic differences among patients treated at trial versus non-trial hospitals in the study of transcatheter tricuspid and mitral valve therapies.
1,050 hospital cardiac surgery programs were included in this study, of which 11.5% (121) had enrolled patients in a relevant clinical trial in 2019. The median number of studies that each trial hospital participated in was 3. Trial hospitals were significantly more likely to be larger in size, located in metropolitan areas, and be teaching centers than non-trial hospitals. Patients undergoing transcatheter valvular procedures at trial hospitals were more likely to reside in higher-income areas than those seeking care at non-trial hospitals. However, the proportion of Black and Hispanic patients at each hospital was not significantly different.
The present study by Nathan et al. sought to determine whether the patient population at trial versus non-trial hospitals amongst cardiac surgery centers participating in transcatheter valvular surgery research differed from a demographic standpoint. They found that trial centers tended to serve a more affluent population but that there were no major differences in the ethnic makeup of the patients. This work suggests that equitable hospital selection for trial participation would do well to ensure that lower-income patients are proportionally represented. A major strength of this study is the large sample size as well as the importance of these results in meeting clinical needs. A primary limitation of this work is the reliance on administrative databases for patient information and the narrow scope of this study to just a small aspect of cardiac surgery practice.
Click here to read this study in JAMA Cardiology
Click to read an accompanying editorial in JAMA Cardiology
Relevant reading: Combating social inequities – diversity, equity and inclusion in clinical and translational research
In-Depth [retrospective cohort]: A retrospective cohort study was conducted using data from the Medicare Beneficiary Summaries, which identified individuals aged 66 or older who were admitted to the cardiac surgery service of participating hospitals in 2019. Standard international disease classification codes were used to further identify patients undergoing a cardiac surgery procedure. Demographic information, including age, sex, ethnic/racial background, geographic location, and socioeconomic status, was gathered. The database ClinicalTrials.gov was used to assess trial versus non-trial hospital designation using relevant search terms for transcatheter valvular procedures.
121 of the 1,050 included hospitals were designated trial centers, each of which participated in a median of three studies (interquartile range 2-5). A p-value <0.001 indicated that trial hospitals were more likely to be teaching centers and to be larger (79.3% vs 30.4% with >400 beds) than non-trial hospitals. Trial hospitals were also more likely to be in metropolitan areas (p=0.03).
Patients undergoing transcatheter valvular procedures at trial hospitals (median income $57,966; interquartile range $44,034-$79,215) were more likely to reside in higher income areas than those seeking care at non-trial hospitals ($50,498; IQR $40,142-$65,422). This difference was statistically significant with p < 0.001. Both unadjusted and adjusted models found that there was a very minimal difference (less than 1%) in the proportion of Black and Hispanic patients admitted to trial versus non-trial hospitals.
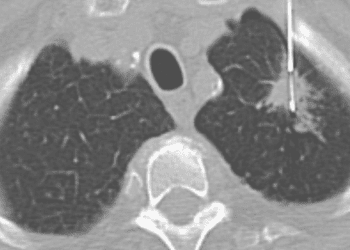
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.