The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]
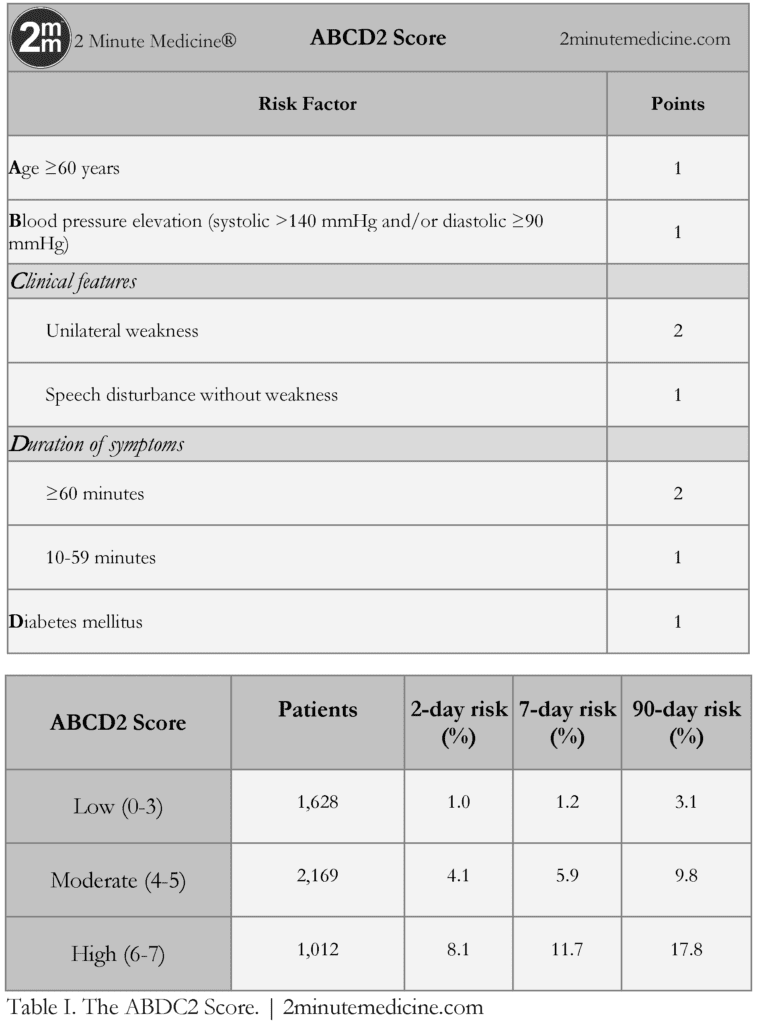
1. The ABCD2 score is a validated, seven-point, risk-stratification tool to identify patients at high risk of stroke following a transient ischemic attack (TIA).
2. Patients with scores ≥4 are at considerably higher risk of stroke in the 2-day period following a TIA, and may potentially require urgent intervention as inpatients.
Original Date of Publication: January 27, 2007
This study summary is an excerpt from the book 2 Minute Medicine’s The Classics in Medicine: Summaries of the Landmark Trials, 2e (The Classics Series).
Study Rundown: The ABCD2 score is a seven-point score for identifying patients who have suffered a transient ischemic attack (TIA) at the highest risk of stroke in the following 2-day period. Since its publication, the ABCD2 score has become widely used by front-line healthcare providers to risk stratify patients with TIA and determine how urgently these patients should be seen for subsequent assessment and treatment. While its c statistic is similar to those of the ABCD and California scores, the ABCD2 score has been more widely validated and has been shown to accurately predict the risk of stroke at 2, 7, and 90 days following a TIA. Some have criticized the ABCD2 score for only taking into account clinical features and not giving any consideration to investigations. Moreover, the score has been shown to be predictive of carotid embolic sources, but less useful for cardiac sources of emboli.
Please click to read study in The Lancet
In-Depth [randomized, controlled study]: Originally published in The Lancet in 2007, the purpose of this study was to develop a tool to identify patients at highest early risk of stroke following a TIA. The ABCD2 score was created by merging two previously validated clinical decision rules – the ABCD and the California scores. The ABCD score was created to estimate the 7-day risk of stroke following a TIA, while the California score predicted the 90-day risk. The two scores shared many features, and were combined in hopes of developing a more widely validated model to identify patients at the highest risk of stroke 2 days after a TIA, thereby allowing clinicians to determine if patients required urgent management.
Study cohorts were drawn from the Kaiser-Permanente Medical Care Plan in Northern California, United States and from Oxfordshire, United Kingdom. The c statistic was calculated to measure predictive ability. All combinations of factors from the ABCD and California scores were tested for their c statistic, and the combination with the highest statistic for 2-day risk of stroke was selected and validated. In total, the two derivation groups and four validation groups included 4,809 individuals with TIA. The new composite score was named the ABCD2 score, because it took into account age, blood pressure, clinical features, duration, and diabetes mellitus diagnoses.
ABCD2 scores were grouped into low-, moderate-, and high-risk categories. The rate of strokes are considerably higher with ABCD2 scores ≥4, and patients who are classified as moderate- and high-risk may require more urgent specialist assessment, investigation, and treatment to prevent stroke.
Johnston SC, Rothwell PM, Nguyen-Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007 Jan 27;369(9558):283–92.
© 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.