The CLARITY trial: Adding clopidogrel to STEMI management [Classics Series]
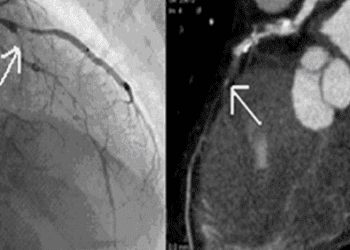
Image: PD
1. The early addition of clopidogrel significantly reduced the incidence of infarct-related arterial re-occlusion within 30 days following myocardial infarction
2. Addition of early clopidogrel improved the outcomes of coronary angiography and decreased the need for early/emergent angiography during the event
3. There were no differences in major or minor bleeding or intracranial hemorrhage incidence between the clopidogrel group and the control group
Original Date of Publication: March 24, 2005
Study Rundown: It is well known that platelet activation and aggregation have a significant role in the initiation and propagation of coronary artery thrombosis. As a result, antiplatelet agents are part of the standard management of acute coronary syndromes. Aspirin, which inactivates the cyclooxygenase enzyme, inhibits platelet aggregation and has been shown to help reduce the rate of reocclusion after myocardial infarction (MI). Clopidogrel is another antiplatelet agent that acts by blocking ADP receptors on platelets. The CLARITY-TIMI 28 trial sought to determine whether early treatment with clopidogrel in addition to standard aspirin and fibrinolytic therapy would produce better outcomes than standard therapy alone in the treatment of ST-elevation MI (STEMI). The study showed that early treatment with clopidogrel had a significant improvement in outcome. The early clopidogrel group had a lower incidence of persistent arterial occlusion or reocclusion, and had improved outcomes on all angiography measures. There was also a significant decrease in the need for early or emergent angiography in the clopidogrel group and a significant decrease in incidence of recurrent MI within 30 days of the first event. No significant difference in 30-day mortality from cardiovascular events was shown, however this study was not powered to assess the impact of intervention on mortality.
In summary, this study showed that early treatment with clopidogrel in addition to standard management of STEMI significantly improves patient outcomes in regard to coronary arterial patency. This study has had meaningful impact on STEMI management and has impacted ACCF and AHA guidelines.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
Study Author, Dr. Marc Sabatine, MD, MPH, talks to 2 Minute Medicine: Chair of the TIMI group, Associate Professor at Harvard Medical School, Cardiovascular Division.
“The results [of this study] helped change clinical practice with the adoption of clopidogrel as part of pharmacologic reperfusion therapy for [patients who present with a] STEMI. Clopidogrel is now part of the standard treatment guidelines for management of a STEMI.
[Now], we are conducting the PEGASUS-TIMI 54 [trial], to sort out the duration of P2Y12 inhibition in patients with ACS.”
In-Depth [randomized, controlled study]: The CLARITY-TIMI 28 trial was a large, multicenter, double-blinded, randomized, placebo-controlled trial that enrolled 3,491 patients with an acute STEMI at 319 sites to receive early clopidogrel or placebo along with standard therapy, including aspirin and fibrinolytic agents. Patients between the age of 18-75 years who presented with ST elevation and an episode of chest pain that lasted >20 minutes within 12 hours of randomization were eligible. Patients who had received clopidogrel in the past 7 days, had a history of coronary artery bypass grafting, presented with cardiogenic shock, or who were scheduled to receive coronary angiography within 48 hours regardless of clinical indication were excluded. Eligible patients received a 300 mg loading dose of clopidogrel followed by 75 mg daily maintenance dose and it was continued up to the day of angiography. If a patient did not undergo angiography, it was continued until day 8 or discharge from hospital, whichever was sooner. Patients were followed up to 30 days after randomization. The primary outcome was evidence of infarct-related arterial occlusion on angiography or death/recurrent MI before angiography, day 8 of hospitalization, or hospital discharge.
The study demonstrated that early treatment with clopidogrel caused a 6.7% absolute reduction of the primary end point (21.7% vs. 15%; 95%CI 24-47%, p<0.001). There was no significant difference in the rate of death from any cardiovascular cause between the two groups. The study also demonstrated no significant difference in incidence of major or minor bleeding or intracranial hemorrhage between the two groups (p=0.64, p=0.17, and p=0.38, respectively).
By Milana Bogorodskaya, Evan Chen, and Andrew Cheung, M.D.
©2012-2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.