The COPERNICUS trial: Beta-blockers in severe chronic heart failure [Classics Series]
1. Adding carvedilol to the management of patients with severe heart failure (NYHA Class III-IV and LVEF<25%) is associated with a 35% relative risk reduction in mortality.
2. In this patient population, carvedilol is also associated with decreased risk of hospitalization and serious adverse effects, as well as improvement in symptoms.
Original Date of Publication: October 2002
Study Rundown: The landmark COPERNICUS trial provided further support to the already established and growing body of evidence supporting the use of beta-blockers in the treatment of heart failure. Prior to COPERNICUS, the randomized controlled trials MOCHA and PRECISE had already demonstrated that carvedilol was associated with reductions in mortality and hospitalizations for patients with mild-moderate heart failure. The COPERNICUS trial, published in Circulation in 2002, investigated the benefit of carvedilol in patients with severe heart failure, defined as NYHA class III-IV and a left ventricular ejection fraction (LVEF) <25%.
Results from this randomized placebo controlled trial showed that carvedilol therapy was associated with a 35% relative risk reduction in mortality. For this reason, the study was terminated 1 year early. Carvedilol was also associated with a similar reduction in the combined risk of death or hospitalization for cardiovascular reasons/heart failure. Patients receiving carvedilol were also significantly more likely to report improvement in symptoms. Furthermore, carvedilol was associated with significantly reduced risk of serious adverse events, including heart failure, sudden death, cardiogenic shock and ventricular tachycardia (45.5% vs. 39.0%).
Please click to read study in Circulation
In-Depth [randomized, controlled study]: The COPERNICUS enrolled a total of 2289 patients. Patients were eligible for the study if they reported symptoms of dyspnea or fatigue at minimal exertion and had a LVEF<25%. These patients were optimized medically on a diuretic and ACE-inhibitor or ARB upon entry to the study. Digitalis, spironolactone, amniodarone and vasodilators were also permitted therapy, but not required for eligibility. Study patients were randomized to receive either 1) carvedilol titrated to a target dose of 25mg BID or 2) placebo. The primary endpoint studied was all-cause mortality. Secondary endpoints were combined risk of death or hospitalization, either due to cardiovascular reason or heart failure, as well as improvement or worsening of symptoms by global patient assessment. Serious adverse events were also studied.
While the study was terminated a year early, patients were followed for a mean of 10.4 months. Results showed that risk of mortality was significantly reduced for those patients receiving (12.8% vs. 19.7%). Equivalent significant risk reductions were observed for number and length of hospitalization as well as the combined secondary endpoints. These effects were consistent in the subgroup analysis, which included sex, age, location, left ventricular function, as well etiology of heart failure (i.e., ischemic vs. non-ischemic). In the global patient assessment, significantly more patients reported moderate to marked improvement in symptoms and were less likely to show moderate to marked worsening. Significantly fewer patients in the carvedilol group experienced serious adverse events, such as worsening of heart failure, sudden death, cardiogenic shock and ventricular tachycardia, as compared to the placebo group.
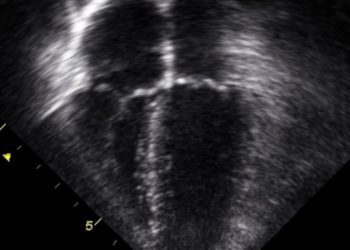
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.