The TORCH trial: Combination of salmeterol and fluticasone in treating COPD [Classics Series]
1. The combination of salmeterol and fluticasone did not significantly reduce all-cause mortality in patients with chronic pulmonary obstructive disease (COPD)
2. When compared with salmeterol alone, fluticasone alone, and placebo, combination therapy significantly reduced the risk of exacerbations and the need for systemic corticosteroids during exacerbations
Original Date of Publication: February 22, 2007
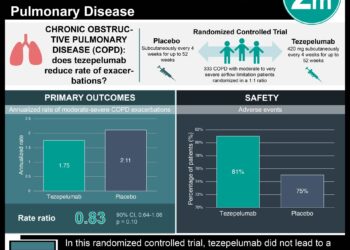
Study Rundown: The Towards a Revolution in COPD Health (TORCH) trial explored whether combination therapy with salmeterol (a long-acting beta-agonist) and fluticasone proprionate (an inhaled corticosteroid) would significantly reduce mortality in patients with COPD as compared with placebo. This landmark study determined that combination therapy did not significantly reduce all-cause mortality when compared with placebo (HR 0.825; 95%CI 0.681-1.002). Treatment with combination therapy, however, did significantly reduce the risk of moderate or severe COPD exacerbations (HR 0.75; 95%CI 0.69-0.81), while also reducing the likelihood that patients would require systemic corticosteroids during their exacerbations when compared with placebo (HR 0.57; 95%CI 0.51-0.64).
In summary, treating patients with COPD with combination therapy including a long-acting beta-agonist and inhaled corticosteroid did not significantly reduce mortality when compared with placebo. This combination therapy, however, does significantly reduce the risk of exacerbation and the risk of requiring systemic corticosteroids for exacerbation treatment.
Click to read the study in NEJM
In-Depth [randomized, controlled study]: Originally published in 2007 in NEJM, this study randomized 6,184 COPD patients to 4 different treatment arms: 1) 1,545 were randomized to the placebo group, 2) 1,542 were randomized to the salmeterol-only group, 3) 1,551 were randomized to the fluticasone-only group, and 4) 1,546 were randomized to the combination therapy group (i.e., salmeterol and fluticasone). Eligible patients had at least a 10 pack-year smoking history, were between 40-80 years old, diagnosed with COPD, exhibited a pre-bronchodilator forced expiratory volume in 1 second (FEV1) of less than 60% of the predicted value, showed an increase in FEV1 with use of 400 mcg of albuterol of less than 10% of the predicted value, and had a ratio of pre-bronchodilator FEV1 to forced vital capacity (FVC) of equal to or less than 0.70. Patients were excluded if they had a non-COPD pulmonary condition (e.g., lung cancer, sarcoidosis, asthma), prior lung volume reduction surgery or lung transplant, long term supplemental oxygen (i.e., greater than or equal to 12 hours/day), less than 6 weeks of oral corticosteroids, serious uncontrolled disease, received any investigational drugs in the 4 weeks prior to entry, evidence of alcohol or drug abuse, known hypersensitivity to inhaled corticosteroids, bronchodilators, or lactose, or known deficiency of alpha-1 anti-trypsin.
There was no significant difference in all-cause mortality between patients in the combination therapy group compared to the placebo group (HR 0.825; 95%CI 0.681-1.002). While there was no significant difference in all-cause mortality when comparing combination therapy with salmeterol-only therapy (HR 0.932, 95%CI 0.765-1.134), combination therapy did significantly reduce all-cause mortality when compared with fluticasone alone (HR 0.774; 95%CI 0.641-0.934). Combination therapy did significantly reduce the risk of moderate or severe exacerbation as compared with salmeterol-only (HR 0.88; 95%CI 0.81-0.95), fluticasone-only (HR 0.91; 95%CI 0.84-0.99), and placebo (HR 0.75; 95%CI 0.69-0.81). Moreover, combination therapy significantly reduced the risk of exacerbations requiring systemic corticosteroids compared to salmeterol-only (HR 0.71; 95%CI 0.63-0.79), fluticasone-only (HR 0.87; 95%CI 0.78-0.98), and placebo (HR 0.57; 95%CI 0.51-0.64).
Image: PD
© 2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.