The VALIANT trial: Valsartan vs. captopril in patients with acute myocardial infarction and heart failure [Classic Series]
1. In patients with acute myocardial infarction and heart failure/evidence of left ventricular dysfunction, patients treated with valsartan and captopril experienced similar all-cause mortality.
2. Valsartan and captopril were found to be non-inferior with regards to death from cardiovascular causes, recurrent myocardial infarction, and hospitalization for heart failure in this patient population.
3. The combination of valsartan and captopril increased the rate of adverse events without improving survival when compared to treatment with captopril alone.
Original Date of Publication: November 2003
Study Rundown: A number of large randomized, controlled trials have previously demonstrated that angiotensin-converting-enzyme (ACE) inhibitors reduced the risk of death and major nonfatal cardiovascular events after myocardial infarction. Angiotensin-receptor blockers (ARBs) represent another way of inhibiting the renin-angiotensin system, and may potentially be more effective than ACE inhibitors in blocking the effects of angiotensin. Moreover, it has been hypothesized that concurrent treatment with an ACE inhibitor and an ARB may be a more effective treatment strategy to reduce the risk of cardiovascular events after a myocardial infarction.
The Valsartan in Acute Myocardial Infarction (VALIANT) trial sought to determine whether valsartan, an ARB, alone or in combination with captopril, an ACE inhibitor, would lead to better outcomes than treatment with an ACE inhibitor alone. This trial found that using valsartan in patients with acute myocardial infarction and heart failure/left ventricular dysfunction resulted in similar all-cause mortality when compared to captopril. Valsartan was found to be non-inferior to captopril for death from cardiovascular causes, recurrent infarction, and hospitalization for heart failure. When comparing combination therapy with captopril alone, there were no significant differences for any of the outcomes. Thus, valsartan is another option for renin-angiotensin blockade in patients with acute myocardial infarction and at high-risk of cardiovascular events.
Click to read the study published in NEJM
In-Depth [randomized controlled trial]: A total of 14 703 patients from 24 countries were randomized in a 1:1:1 ratio to treatment with valsartan only, captopril only, or a combination of the two. All patients 18 years of age or older, with acute myocardial infarction (0.5-10 days prior to randomization) complicated by clinical or radiographic heart failure, left ventricular dysfunction (ejection fraction ≤35% on echocardiogram, ≤40% on radionuclide ventriculography), or both were eligible for the trial. Patients were excluded if they had systolic blood pressure <100 mmHg, serum creatinine <2.5 mg/dL (or 221 μmol/L), intolerance or contraindication to ACE inhibitor or ARB, clinically significant valvular disease, or another disease known to limit life expectancy. The primary outcome was all-cause mortality, while the secondary outcome was a composite of death from cardiovascular causes, recurrent myocardial infarction, or hospitalization for heart failure.
The median follow-up was 24.7 months. There was no significant difference between the valsartan and captopril groups in all-cause mortality (HR 1.00; 97.5%CI 0.90-1.11; p = 0.98). All-cause mortality was also found to be similar when comparing combination therapy with captopril alone (HR 0.98; 97.5%CI 0.89-1.09; p = 0.73). The three groups were also similar in terms of the rate of the secondary endpoint, with no significant differences between valsartan and captopril (HR 0.95; 97.5%CI 0.88-1.03; p = 0.20) or between combination therapy and captopril (HR 0.97; 97.5%CI 0.89-1.05).
The discontinuation rates were significantly higher in the combination group, as compared with captopril alone (19.0% vs. 16.8%, p = 0.007). Dose reduction for hypotension was significantly more common in the combination and valsartan groups when compared with the captopril group (18.2%, 15.1%, and 11.9%, respectively; p < 0.05). There were also significantly higher rates of permanent discontinuation of therapy due to adverse events in the combination group when compared to captopril alone (9.0% vs. 7.7%; p < 0.05).
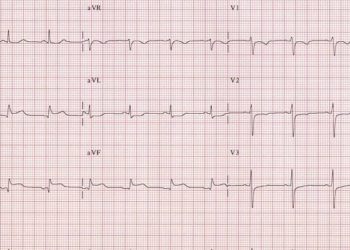
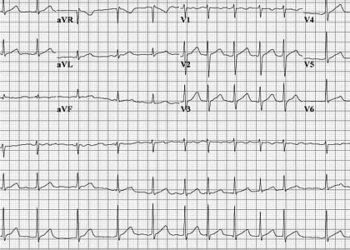
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.