Thromboelastography velocity better for predicting hyperfibrinolysis in trauma
1. Large volume transfusion requirement and mortality in trauma are better predicted using clot lysis velocity curves.
2. Pathological hyperfibrinolysis can be predicted earlier in trauma using the maximum rate of lysis (MRL) which may facilitate earlier decision making at no additional cost.
Evidence Rating Level: 2 (Good)
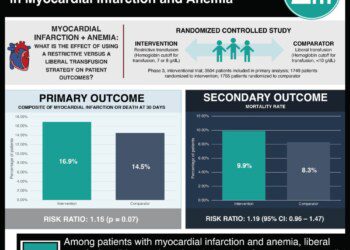
Study Rundown: In acute trauma hyperfibrinolysis represents a pathological response that leads to excessive clot breakdown, coagulopathy and increased bleeding with transfusions. Rapid thromboelastography (rTEG) is a technique used to measure the efficacy of blood coagulation and is able to assess platelet function, clot strength, and fibrinolysis which standard tests such as INR and PTT cannot. Traditionally, hyperfibrinolysis, as measured by rTEG, has been used to predict post-injury transfusion needs and mortality risk.
In this retrospective review of 1625 patients’ care, conventional rTEG values were compared with first derivative velocity curves of rTEG, measuring MRL and total lysis (TL). The primary study outcomes included the predictive value of early transfusion, substantial bleeding, massive transfusion, and mortality. The predictive value of clot strength surrogates, LY30 which looks at the percent of a clot that has broken down after 30 minutes, and the maximum rate of lysis (MRL) were investigated. Authors found that velocity curves of MRL were more predictive of massive transfusion risk and mortality risk than standard MRL or LY30 values.
The strengths of this study were the use of established study methods using rTEG to find better predictive values, the significant power, and multivariate analysis to reduce confounders. The study was limited by its retrospective nature and the use of single institution data. Despite these limitations, this study demonstrates the utility of rTEG velocity curves to establish MRL and TL values that are faster and more predictive of hyperfibrinolysis at no additional cost.
Click to read the study in The Journal of the American College of Surgeons
Relevant Reading: Initial experiences with point‐of‐care rapid thrombelastography for management of life‐threatening postinjury coagulopathy
In-Depth [retrospective cohort]: Patients selected for this study were seen over an 18-month period between 2009 and 2011 at a high volume shock-trauma ICU in Houston, TX. Patients were excluded if they were under 18 years of age, had burns >20% body surface area, or died within 30 minutes of arrival. Hyperfibrinolysis was defined as LY30 >3%, corresponding to a 2-fold increase in mortality. Using derivative velocity curves, hyperfibrinolysis was defined as MRL >0.5mm/min and TL>60mm reduction in amplitude. Multimodal analysis was used to stratify patients based on age, gender, mechanism of injury, weighted revised trauma score, injury severity score, shock index and base value.
The patients were predominantly young to middle aged males suffering blunt trauma and 29% of total patients arrived in septic shock. Overall 30 day mortality was 11% and 24 hour mortality was 5. 11% of all patients met criteria for hyperfibrinolysis using LY30 cutoffs vs. 9% using MRL cutoffs. In contrast to LY30 cutoffs of hyperfibrinolysis, which were associated with massive transfusion risk only, velocity curves (for both MRL and TL) were more predictive of massive transfusion risk (18.3% vs 12.0%: p<0.001) as well as significant bleeding. Twenty-four hour mortality risk was 10-fold higher with MRL cutoffs vs. 3-fold increases using LY30 cutoffs. Similarly, velocity curves were more predictive of 30-day mortality as well (24.4% vs. 18.0%; p<0.001). Additionally, MRL values were available 13 minutes earlier (32 minutes upon arrival) than LY30 (45 minutes upon arrival).
More from this author: Previous stroke may increase risk of complications after major surgery, Patient-controlled pain meds superior to epidural after laparoscopic surgery, Weight loss before gastric bypass may reduce post-operative complications
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.