Ultrasound-guided cryoablation shows promise in treating ductal carcinomas
1. Ultrasound-guided cryoablation of invasive ductal carcinomas up to 15 mm in size was technically feasible, well-tolerated by patients, and largely clinically successful, as assessed by negative surgical margins following the procedure. However, a significant portion of patients had residual peripheral cancer.
2. Postablation contrast-enhanced magnetic resonance imaging was performed to assess procedural success, but was insensitive in detecting residual malignancy, and therefore an unreliable predictor of postablative outcomes
Evidence Rating: 4 (Below Average)
Study Rundown: Cryoablation has successfully been used to treat fibroadenomas and aid in surgical excision, but has had limited results in the treatment of breast cancer. However, it remains an attractive strategy in the management of breast cancer as it is minimally invasive, is performed in the office, and may potentially allow for avoidance of invasive surgery. The current study sought to pilot the viability of ultrasound-guided cryoablation as the definitive management of small (up to 15 mm) invasive ductal carcinomas (IDC), hypothesizing that the small tumor size may be more amenable to such treatment. Additionally, the authors tested the efficacy of contrast-enhanced magnetic resonance imaging (CE-MRI) in evaluating the postablative tumor bed for procedural success as compared against the gold standard of a surgical resection. Although the procedure was well-tolerated and technically feasible in all patients, it was not clinically successful in 15% of patients with residual cancer detected on surgical resection of the cryoablation site. Postablation CE-MRI had a 0% specificity in identifying residual malignant tissue at and around the ablation site, and a specificity of 88%, incorrectly identifying benign tissue as a potential malignancy in two patients. This pilot study helped establish tumor characteristics that may be most amenable to cryoablative therapy in light of previous research, while determining the feasibility of the procedure and identifying its clinical limitations in the treatment of breast cancer. Additionally, it showed that CE-MRI may not be an appropriate post-procedural follow-up study, highlighting a future research avenue for a more specific imaging modality. The study was limited primarily by its design: a case-series with a small sample size makes broad applicability of its findings untenable, though it does identify cryoablation as a viable procedure for continued clinical study. Future studies should aim to further test the size and tumor types that may be effectively treated by ultrasound cryoablation with a larger sample size, while testing alterative imaging modalities for superior evaluation of the postablative tumor bed for residual disease.
Click to read the study in American Journal of Roentgenology
Relevant reading: Cryotherapy for breast fibroadenomas
In-Depth [case series]: This study enrolled 20 consecutive patients at 2 different sites with known, pathologically proven invasive ductal carcinomas up to 15mm in size. All patients underwent preablation mammography, ultrasound, and CE-MRI to ensure unifocal disease and tumor size for eligibility determination. Patients were followed for a 2-week period following cryoablation, specifically evaluating for evidence of hematoma, infection, or thermal injury at the ablation site. Following ablation, all patients underwent CE-MRI to evaluate for residual disease at 25-40 days, followed by surgical resection. Lumpectomy was performed in 19/20 of patients and mastectomy (independent decision) in 1/20, with results compared to post-procedural CE-MRI as a reference standard. At surgical resection, 15% (3/20) of patients had residual cancer found in the periphery of the cryoablation site, while 10% (2/20) had viable nonmalignant tissue within the central zone of the ablation bed, denoting an incomplete ablation. Postablation CE-MRI detected 0 of 3 residual malignancies with a resultant sensitivity of 0%, while it falsely identified 2 benign masses as potential malignancies for a specificity of 88% (15/17 studies correctly identified as negative.) The calculated negative predictive value of CE-MRI was found to be 83% (15/18). There were no differences in cancer characteristics, cryoablation procedural variables, postablation CE-MRI findings, or patients with or without residual cancer, and all patients tolerated the procedure without incident and with minimal anesthetic requirements.
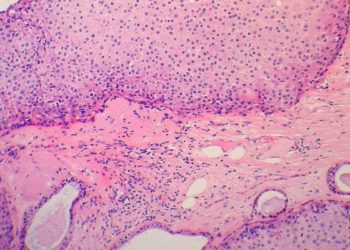
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.