Unclear utility of the European Society of Cardiology 0/1h troponin algorithm in diagnosing acute coronary syndrome in patients with known coronary artery disease
1. The negative predictive value for the ESC 0/1h troponin algorithm was lower in patients with known coronary artery disease than those without.
2. The ESC 0/1h algorithm could not safely exclude acute coronary syndrome within 30 days in patients with coronary artery disease and should be interpreted with caution.
Level of Evidence Rating: 2 (Good)
Study Rundown: Cardiac troponin is an important clinical biomarker of myocardial insult, used in the context of a patient’s clinical presentation to diagnose acute coronary syndrome (ACS). The European Society of Cardiology (ESC) has developed an algorithm to rule out non-ST elevation myocardial infarction based solely on troponin levels. Previous studies of this algorithm have found it to have a negative predictive value of 99% or higher. However, the algorithm is not designed to differentiate between patients with, and without known coronary artery disease (CAD), despite CAD being a leading risk factor for ACS. This study sought to compare the diagnostic performance of the ESC 0/1h algorithm in patients with and without known CAD.
1430 patients were included in this study, of which 449 (31.4%) had CAD. The primary outcome occurred in 183 (12.8%) patients. Significantly more patients with CAD experienced cardiac death or myocardial infarction than patients without CAD. The ESC 0/1h algorithm was significantly more likely to miss the primary outcome in patients with CAD than those without CAD at 30 days. The negative predictive value for 30–day cardiac death or myocardial infarction was 96.6% in patients with CAD and 98.9% in those without CAD. However, the algorithm’s sensitivity was similar in patients with and without CAD. The proportion of patients misassigned by the algorithm as false positives were similar between CAD and non-CAD patients.
This study by Ashburn et al. demonstrated differences in the diagnostic utility of the ESC 0/1h troponin-based algorithm in patients with and without a history of coronary artery disease. It was significantly more likely to miss ACS events within 30 days amongst patients with a history of CAD, and the calculated negative predictive value was below the predetermined acceptable value of 99%. As such, the recommendations from this algorithm should be interpreted with caution, particularly amongst patients with a history of CAD. One limitation of this study is the low external validity given that the patient population was derived from only academic hospitals in the United States.
Click here to read this study in JAMA Cardiology
Relevant reading: Myocardial infarction risk stratification with a single measurement of high sensitivity troponin I
In-Depth [prospective cohort]: This study represents an a priori, planned analysis of the larger High Sensitivity Cardiac Troponin T to Optimize Chest Pain Risk Stratification cohort study. Patients older than 21 with chest pain, or other symptoms of ACS, and available serial troponin readings, were enrolled at several American medical centers. Patients who were hemodynamically unstable (systolic blood pressure <90mmHg), non-English speaking, pregnant, or had a life-limiting illness and life expectancy under 90 days were excluded. History of CAD included: previous myocardial infarction, coronary revascularization or coronary stenosis >70%. Serum troponin levels were collected at baseline and 1 hour for study purposes, in addition to clinical values. The primary outcome was 30-day cardiac death or myocardial infarction.
19.6% of patients with CAD experienced an MI or cardiac death, whereas 9.7% of those who did not have CAD did. This difference was statistically significant (p<0.001). As per the ESC 0/1h algorithm, 39.6% of patients with CAD and 66.1% of patients without CAD were ruled out of having ACS. At 30 days, 3.4% of the “ruled-out” CAD patients and 1.1% of the “ruled-out” non-CAD patients had experienced the primary outcome, representing false negatives by the algorithm’s designation. The odds ratio for a false negative in the CAD versus non-CAD group was 3.9 (95% confidence interval 1.05-9.63).
The algorithm’s sensitivity to detect the primary outcome was 93.2% (85.7-97.5%) in patients with CAD and 92.6% (85.4-97.0%) in those without CAD. The positive likelihood ratio was lower for patients with CAD (5.9, 4.2-8.5) than those with known CAD (12.8, 9.2-17.8).
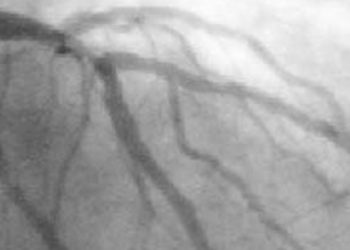
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.