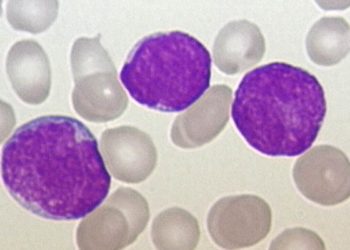
Universal decolonization effective at reducing MRSA
Image: PD
1. Universal decolonization of ICU patients was superior to targeted decolonization. It reduced the likelihood of MRSA infection in the ICU by 37% and reduced the risk of any bloodstream infection by 44%.
2. Universal decontamination can be adopted by most hospitals, as the effects of universal decontamination were observed under usual practice and with the existing infrastructure of a wide array of hospitals.
Evidence Level: 1 (Excellent)
Study Rundown: Several factors likely contributed to the reduction in infections seen with universal decolonization: the reduction of skin colonization by pathogens, reduction of environmental microbial burden, and immediate implementation of decolonization upon admission to the ICU. This study also highlights two important issues: (1) MRSA screening delays decolonization of carrier patients and (2) contact precautions can impede patient care. Universal decolonization may be sufficiently effective to obviate the need for contact precautions and may speed the treatment of MRSA-carriers by removing standardized screening. Bacterial resistance to chlorhexidine and muciporin has been documented, but is of unknown clinical significance. As a result, in conjunction with universal decolonization the authors cite the need for vigilant monitoring of emerging resistance. Importantly, this study was implemented with the existing infrastructure of a wide array of hospitals therefore could be implemented in most hospitals across the United States.
Click to read the study in NEJM
In-Depth [cluster randomized trial]: The study was conducted in 43 hospitals across America andcompared universal decolonization, screening and targeted decolonization, and screening and isolation of ICU patients. For universal decontamination patients were started immediately on five days of intranasal mupirocin and daily chlorhexidine baths upon ICU admission. For targeted decontamination, MRSA-positive patients received 5 days of chlorhexidine and mupirocin. In the final group, patients were screen and put on standard contact precautions if MRSA positive. Universal decolonization resulted in a greater reduction in MRSA positive cultures (hazard ratio 0.63; 95% CI 0.52 to 0.75) than screening and isolation (hazard ratio 0.92; CI 0.77 to 1.10; P=0.003). Though not significantly different between groups, MRSA-bloodstream infections were lowest in the universal decolonization group. However, bloodstream infection from any pathogen was significantly lower in this group (hazard ratio of 0.56; (CI0.49 to 0.65).
By Jessica Mitchell and Mitalee Patil
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.