#VisualAbstract: Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy
1. Anticoagulation at prophylactic dosing appeared to be associated with lower mortality and better prognosis in COVID-19 patients with coagulation dysfunction: i.e., sepsis-induced coagulopathy or a D-dimer greater than 6 times the upper limit or normal (30ug/mL).
2. No mortality benefit was found between heparin users and nonusers in other groups.
Evidence Rating: 3 (Average)
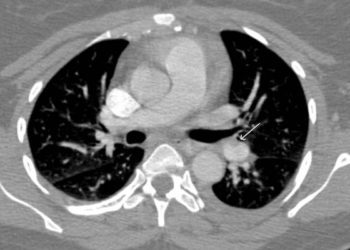
Anticoagulation initiation for COVID-19 patients has been a topic of discussion and recommended by some clinicians due an increased risk of disseminated intravascular coagulation / sepsis-induced coagulopathy (SIC) and venous thromboembolism, though its efficacy has not been validated. This retrospective cohort study reviewed data from 449 patients with severe COVID-19 admitted to the Tongji Hospital of Huazhong University of Science and Technology between January 1 to February 13, 2020. One hundred and eighty-one females and 268 males were included, with a mean age at disease onset of 65.1 years. Ninety-nine (22%) patients had received heparin therapy at prophylactic dosing for at least 7 days, 94 of which received LMWH (40-60mg enoxaparin daily), and 5 who received UFH (10000-15000 U daily). No other anticoagulants were used for more than 7 days for any patients. Despite all patients having received antiviral and appropriate medical management, 134 (29.8%) of patients had died by March 13, 2020. A positive correlation between D-dimer, prothrombin time, and age, was found with 28-day mortality, whereas platelet count was negatively correlated with mortality. Compared to nonusers, patients on prophylactic therapy had essentially equivalent rates of mortality. However, significant reduction in mortality rates were observed in patients with coagulopathy, as defined by a SIC score of >3 (40% vs. 64.2%, P = .029) or D-dimer exceeding 3.0ug/mL (32.8% vs. 52.4%, P = .017). Study findings appear to suggest a potential role of anticoagulation in COVID-19 patients with coagulation dysfunction representing an important therapeutic strategy in reducing overall mortality for the disease. Nonetheless, the effectiveness of prophylactic dosing of anticoagulation for sepsis-associated coagulopathy appears to be controversial even beyond the scope of COVID-19 patients, and as such, further validation in clinical trials is needed to better characterize its efficacy.
Click to read the study in Journal of Thrombosis & Haemostasis
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.