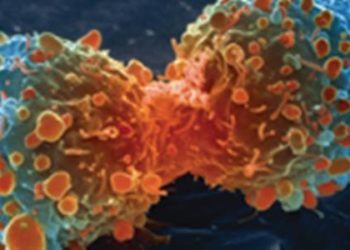
#VisualAbstract: Atezolizumab may increase overall survival in patients with metastatic non-small-cell lung cancer
1. Atezolizumab significantly increased overall survival compared to platinum-based combination chemotherapy in participants with untreated metastatic non-small-cell lung cancer (NSCLC) and high programmed death 1 ligand (PD-L1) expression.
2. Atezolizumab was associated with longer progression-free survival compared to platinum-based combination chemotherapy.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The first line-treatment for advanced non-small-cell lung cancer (NSCLC) without mutations is inhibitors to programmed death 1 (PD-1) and its ligand PD-L1. Atezolizumab, an anti-PD-L1 monoclonal antibody, shows an overall survival benefit in participants with high PD-L1 expressing NSCLC tumors in Phase 2 studies. Even with the advances in treatment for metastatic NSCLC, additional treatments are needed. As such, this Phase 3 study evaluated the atezolizumab monotherapy in comparison to platinum-based chemotherapy for PD-L1 selected participants with metastatic NSCLC. The study results demonstrated that atezolizumab treatment significantly increased overall patient survival compared to platinum-based chemotherapy among participants with high PD-L1 expressing NSCLC tumors, regardless of histologic type. This randomized trial was limited by the additional biomarker analysis. The trial selected for participants with any expression level of PD-L1 from one particular assay. Therefore, additional biomarker analysis resulted from a double-selected patient population. Nonetheless, the results are significant, and the findings highlight the benefit of a different medication for participants with few treatment options.
Click to read the study in NEJM
Relevant Reading: Pembrolizumab plus chemotherapy for squamous non–small-cell lung cancer
In-Depth [randomized controlled trial]: This study enrolled 572 participants in a multicenter study at 144 locations in 19 countries. Participants included in the study had stage IV nonsquamous or squamous NSCLC, no previous chemotherapy, and PD-L1 expression on at least 1% of tumor cells or tumor-infiltrating immune cells as determined by the SP142 assay. Participants with known epithelial growth factor receptor (EGFR) mutation of anaplastic lymphoma kinase (ALK) translocation were excluded from this study. The participants were randomized in a 1:1 ratio to receive 1200 milligrams, intravenously, of atezolizumab or 4 to 6 cycles of platinum-based chemotherapy every 3 weeks, respectively. The primary end point was overall survival. The median follow-up time for survival among participants with high PD-L1 expression was 15.7 months (range, 0 to 35). Among participants with high PD-L1 expressing tumors, the median overall survival in the atezolizumab group was significantly longer at 20.2 months compared to 13.1 months in the chemotherapy group (difference, 7.1 months; hazard ratio, 0.59; 95% confidence interval [CI], 0.40 to 0.89; P=0.01). In the subgroup with high or intermediate PD-L1 expressing tumors, the median overall survival between the two groups was not significant (atezolizumab group, 18.2 months; chemotherapy group, 14.9 months; hazard ratio, 0.72; 95% CI, 0.52 to 0.99; P=0.04). Similarly, there was no significant difference in the median overall survival between the two group with tumors that were not formally tested for PD-L1 expression (atezolizumab group, 17.5 months; chemotherapy group, 14.1 months; hazard ratio, 0.83; 95% CI, 0.65 to 1.07). At the end of follow-up, 146 of the 205 participants (71.2%) with high PD-L1 expressing tumors had disease progression or died. However, progression-free survival in the atezolizumab group was 8.1 months compared to 5.0 months in the chemotherapy group (hazard ratio, 0.63; 95% CI, 0.45 to 0.88). Finally, the safety analysis determined adverse events occurred in 90.2% of participants in the atezolizumab group and 94.7% of participants in the chemotherapy group. Specifically, Grade 3 or 4 adverse events occurred in the 30.1% of participants in the atezolizumab group and 52.5% of participants in the chemotherapy group with anemia, neutropenia, and thrombocytopenia being the most common. Taken together, atezolizumab monotherapy significantly increased overall survival in participants with high PD-L1 expressing metastatic NSCLC.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.