#VisualAbstract: Continuous infusion of hypertonic saline following traumatic brain injury does not improve neurological outcomes versus current standard of care
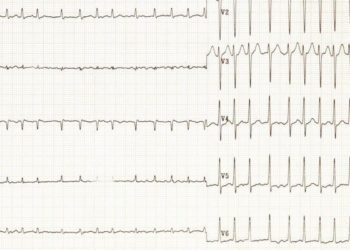
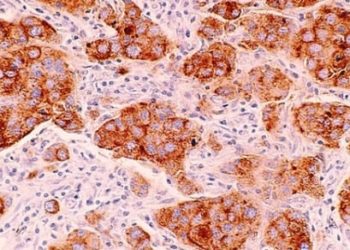
1. No significant difference was found in neurological function recovery measured by extended Glasgow scale score in patients with moderate to severe traumatic brain injury 6-months after treatment with either continuous hypertonic saline or current care protocol.
2. No significant different in 6- month mortality was found between continuous hypertonic saline and current care protocols.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The prevalence of disability after traumatic brain injury continues to be high, despite mortality after injury decreasing over the previous decades with new interventions. A contributing factor to the plateau in traumatic brain injury-related disability comes from intracranial hypertension (ICH) and the difficulties associated with its management. This study compared intracranial hypertension risk, along with neurological function and autonomy 6-months after moderate to severe TBI, when treated with either continuous hypersaline solution (0.5-1g/h of NaCl) or Brain Trauma Foundation standard care guidelines. Neurological function and autonomy were determined using the extended Glasgow scale (GOS-E), which is a validated scale that assigns a score from 1-8 depending on the person’s ability to perform daily activities with 8 representing high functioning individuals and 1 being death. The study randomized 370 patients to either being treated with continuous hypersaline solution or standard care (i.e., the Brain Trauma Foundation standard of treatment), so each group had a population size of 185. Experimental groups were similar in age, sex, baseline consciousness, rate of hypoxia, and time from trauma event. After patients were examined 6 months after TBI, percentage of favourable GOS-E scores were not significantly different between the groups. Individuals treated with continuous hypersaline solution had 59 individuals (32.6%) with scores between 6 and 8 while the standard care group had 63 individuals (35.4%) with scores 6-8. There was also no significant difference in the prevalence of developed ICH, as the hypersaline group had an ICH rate of 33.7%, while the standard care group had an ICH rate of 36.3%. These results suggest that neither continuous infusion of hypersaline solution or current Brain Trauma Foundation standard care is more superior than the other in the prevention of ICH. These results are aligned with current research, as it is still unclear if standard care involving the use of mannitol or using hypersaline solution is more superior to the other. An important finding in this study to note was that continuous hypersaline solution did show a significant decrease in the risk of ICH, but only for the first 4 days after intervention. This indicates a plausible blood pressure rebound effect, and may indicate that more research is required in the discontinuation of hypertonic solution to lengthen its plausible effect. A limitation to this study is the standard care group also received hyperosmolar therapy if needed, which is a confounding variable and may be a reason for the neurological recovery in the standard care group. The study was methodologically sound, with one strength in particular being the use of equal experimental group populations and randomizing them using an independent statistician.
Click to read the study in JAMA
In-Depth [randomized controlled trial]: This randomized control trial compared intracranial hypertension risk and neurological recovery 6 months after traumatic brain injury when treated with either current Brain Trauma Foundation standard treatment guidelines or continuous 20% NaCl saline solution. Brain Trauma Foundation treatment involved the use of isotonic crystalloids for maintenance and first-line resuscitation strategies. The study took place across 9 different hospitals in France from October 2017 to February 2020. The study quantified neurological recovery using extended Glasgow Outcome scores of 6-8 as favourable and 5-1 as unfavourable. The study also assessed for the presence of intracranial hypertension, along with mortality, amnesia, electrolyte abnormalities, acute kidney injury, deep vein thrombosis, pulmonary emboli, and hospital-acquired pneumonia. The two experimental groups consisted of 185 individuals 18-80 years in age with moderate to severe TBI. The hypertonic saline solution group had a mean age of 46 with a 78.8% male population. The standard care group had a mean age of 43 with an 80.9% male population. Care was initiated 13 hours on average (8-18 hours) after injury in the hypertonic saline group and 12 hours on average (7-18 hours) in the standard care group. Interventions were continued for a minimum of 48 hours, and were planned to be monitored for 48 hours after intervention. However, individuals who received continuous hypertonic saline needed to be monitored longer as resulting hypernatremia needed longer to normalize. Hypertonic saline solution therapy did show a significant reduction in ICH in the first 4 days after cessation of intervention, but after 6 months the reduction of risk of ICH was not significantly different to standard care. The standard care therapy group had 16 individuals who had a GOS-E score of 8, 18 individuals who scored a 7, and 29 individuals who scored a 6 for a total of 63 people who had favourable GOS-E scores. This was similar to the individuals treated with hypertonic saline solution, as this group had 9 individuals who scored an 8, 23 individuals who scored a 7, and 27 individuals who scored a 6 for a total of 59 people who had favourable GOS-E scores. Intracranial hypertension was also not significantly different between groups, as 62 (33.7%) individuals developed ICH when treated with continuous hypertonic solution and 66 (36.3%) individuals developed ICH when treated with standard care (absolute difference, −2.6% [95%CI, −12.3%to 7.2%]; Odds Ratio, 0.80 [95% CI, 0.51-1.26]). These results show that hypertonic saline solution is comparable in treating ICH to current standard care therapy. However, this study showed standard care may be superior over hypertonic saline solution, as hypertonic saline solution had a significantly higher rate of hypernatremia, 23% and 11% for hypertonic saline solution and standard care therapy respectively. There were no other significant differences in mortality, amnesia, electrolyte abnormalities, acute kidney injury, deep vein thrombosis, pulmonary emboli, and hospital-acquired pneumonia.
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.