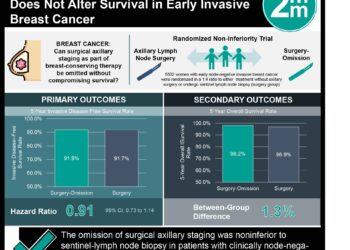
#VisualAbstract: Pembrolizumab plus chemotherapy improves survival in patients with metastatic triple-negative breast cancer
1. First line treatment with pembrolizumab-chemotherapy showed significant improvement in progression-free survival compared to chemotherapy alone in patients with metastatic triple-negative breast cancer and a CPS of 10 or more.
2. There was no significant increase in adverse events or death with the addition of pembrolizumab to standard first-line chemotherapy.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Triple-negative breast cancer is challenging to treat due to the absence of targets for therapeutic intervention. Cytotoxic chemotherapy remains the standard treatment for most patients, but these tumours become rapidly resistant to chemotherapy. Pembrolizumab is an anti-PD-1 monoclonal antibody which has shown promising anti-tumour activity across many tumour types with an acceptable safety profile. This randomized controlled phase 3 clinical trial aimed to evaluate the efficacy and safety of pembrolizumab plus chemotherapy to chemotherapy alone in patients with previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer. Results suggested that pembrolizumab-chemotherapy resulted in significant, clinically meaningful improvements in progression-free survival compared to chemotherapy alone in patients with CPS ≥10. The benefits on progression-free survival were consistent across pre-defined subgroups including type of chemotherapy and disease-free interval. Treatment related adverse event rates were similar between groups. A key strength of the current study comes from its inclusion of both taxanes and platinum-based chemotherapy regimens allowing for the assessment of pembrolizumab in combination with different chemotherapy agents. However, the subgroup analysis showing persistent benefit of pembrolizumab irrespective of chemotherapy partner was underpowered and, as such, the results of subgroup analysis should be interpreted with caution.
Click to read the study in The Lancet
Relevant Reading: Pembrolizumab for Early Triple-Negative Breast Cancer
In-Depth [randomized controlled trial]: This randomized, placebo-controlled, double-blind, phase 3 clinical trial done in 209 sites in 29 countries around the world included adults aged >18 years of age with untreated locally recurrent inoperable or metastatic triple-negative breast cancer. Participants were randomized to pembrolizumab (200 mg) every 3 weeks plus chemotherapy (one of nab-paclitaxel, paclitaxel, or gemcitabine plus carboplatin) or placebo plus chemotherapy. Randomization was stratified by type of chemotherapy, PD-L1 expression at baseline (combined positive score (CPS) ≥1 or <1), or previous treatment by the same class of chemotherapy in adjuvant or neoadjuvant setting. The primary efficacy endpoints of this study were progression-free survival and overall survival in the intention-to-treat and subgroup analysis.
A total of 847 patients (median age=53) were randomly assigned to treatment with 566 patients in the pembrolizumab-chemotherapy group and 281 patients the placebo-chemotherapy group. Overall, among patients with CPS ≥10, median progression-free survival was 9.7 months on pembrolizumab-chemotherapy compared to 5.6 months on placebo-chemotherapy (hazard ratio [HR] for progression or death 0.65, 95% CI 0.49 to 0.86; p=0.0012). In patients with CPS of 1 or more, median progression-free survival was 7.6 months in the pembrolizumab-chemotherapy group and 5.6 months in the placebo-chemotherapy group (HR 0.74, 95% CI 0.61 to 0.90; p=0.0014 [not significant]). Adverse events considered to be related to study treatment occurred in 96% of patients in the pembrolizumab-chemotherapy group compared to 95% in the placebo-chemotherapy group with anemia (49% vs. 46%), neutropenia (41% vs. 38%) and nausea (39% vs. 41%) being the most common side effects noted. Death occurred in <1% of the pembrolizumab-chemotherapy group compared to 0% in the placebo-chemotherapy group.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.