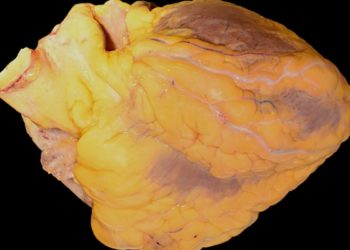
#VisualAbstract: Rilonacept may lower pericarditis recurrence in patients with relapsing pericarditis
1. Rilonacept significantly lowered pericarditis recurrence risk compared to placebo.
2. Rilonacept rapidly resolved recurrent pericarditis episodes in at risk patients.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Recurrent pericarditis is characterized by chronic and debilitating pericardial inflammation with limited treatment options such as glucocorticoids. However, the nonspecific immunosuppression property of glucocorticoids is particularly concerning for long-term use. Alternatively, interleukin-1 inhibition is a potential therapeutic for patients with systemic inflammation including pericarditis. As such, this study evaluated whether rilonacept, an interleukin-1α and interleukin-1β cytokine trap, could reduce the risk of pericarditis recurrence. The study determined rilonacept significantly lowered pericarditis recurrence risk, while rapidly resolving pericarditis episodes. The randomized control trial was limited by the randomized-withdrawal trial study design. Nonetheless, this study’s results are significant, and its findings highlight an effective treatment reduce recurrent pericarditis risk in patients with rilonacept treatment.
Click to read the study in NEJM
Relevant Reading: Effect of Anakinra on Recurrent Pericarditis Among Patients with Colchicine Resistance and Corticosteroid Dependence: The AIRTRIP Randomized Clinical Trial
In-Depth [randomized controlled trial]: This randomized-withdrawal trial enrolled 86 participants in a multicenter study in four countries. Participants included in the study were ≥ 12 years of age with recurrent pericarditis, presented with pericarditis during at least a second recurrence, and received combinatorial treatment of nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, or glucocorticoids. Participants with a pain score of less than 4 on a numerical rating scale were excluded from this study. The participants were randomized in a 1:1 ratio to weekly receive rilonacept or placebo, respectively. The primary endpoint was recurrence events. A recurrence event was defined as return of pericarditis pain and an increased in C-reactive protein (CRP) levels. During the run-in period, the median time to pain response was 5 days (95% confidence interval [CI], 4 to 6) and the median time to CRP level normalization was 7 days (95% CI, 5 to 8). Out of the enrolled 86 participants, 61 participants completed the run-in period and underwent randomization. At the end of the randomized-withdrawal period, rilonacept led to a significantly lower pericarditis recurrence risk compared to the placebo (hazard ratio, 0.04; 95% CI, 0.01 to 0.18; P<0.001). During this period, 2 of 30 participants (7%) in the rilonacept group had a pericarditis recurrence compared to 23 of 31 patients (74%) in the control group. Additionally, 17 of 21 participants (81%) had a persistent clinical response at 16 weeks in the rilonacept group compared to 4 of 20 participants (20%) in the control group (difference, 61; 95% CI, 37 to 85; P<0.001). Furthermore, 17 of 21 participants (81%) presented with absent or minimal pericarditis symptoms in the rilonacept group compared to 5 of 20 participants (25%) in the control group (difference, 56; 95% CI, 31 to 81; P<0.001). Finally, injection-site reactions and upper respiratory tract infections were the most common adverse events. Overall, 29 participants (34%) and 7 participants (23%), all whom received rilonacept, had injection-site reactions and upper respiratory tract infections, respectively. Taken together, rilonacept significantly lowered the risk of pericarditis recurrence in at-risk patients.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.