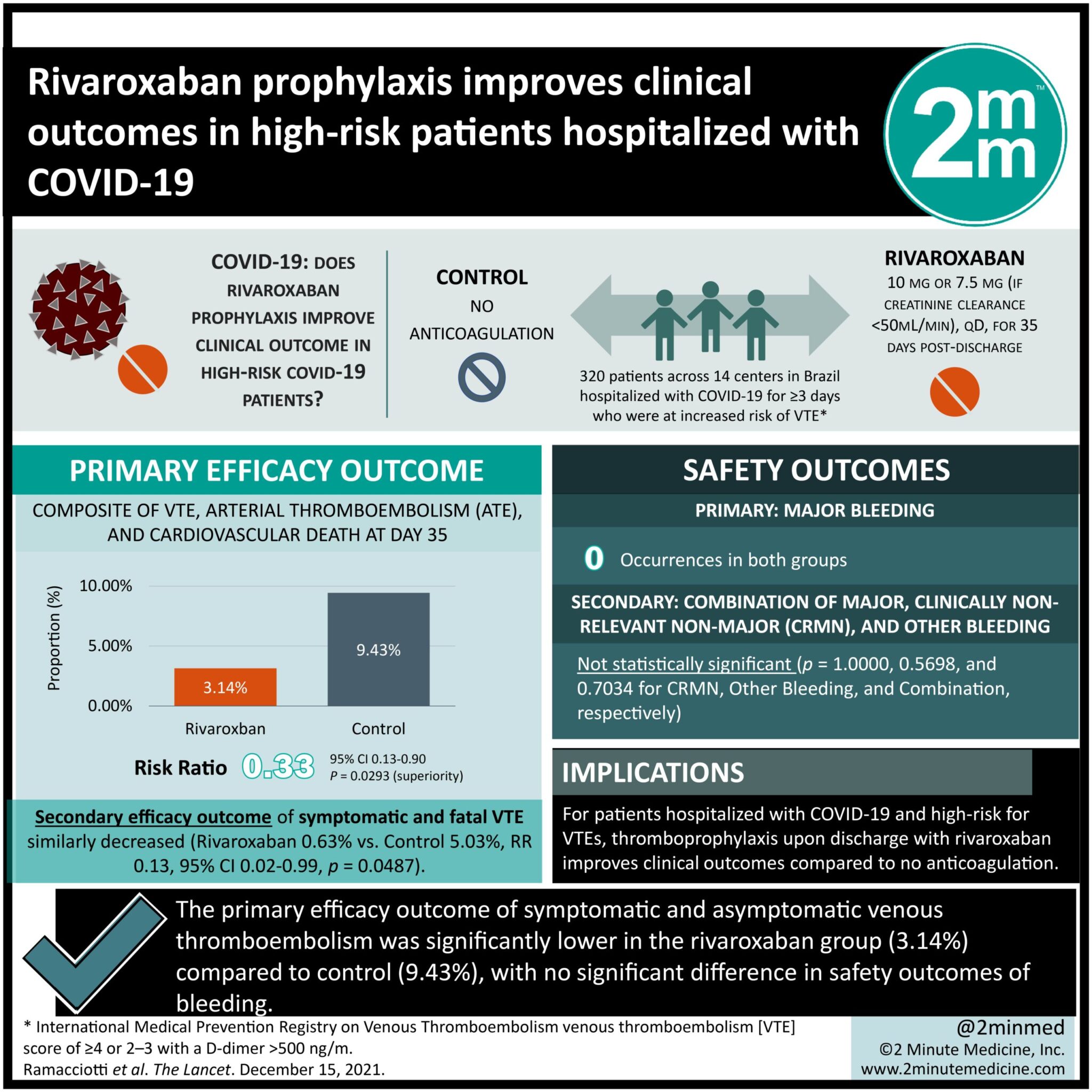
#VisualAbstract: Rivaroxaban prophylaxis improves clinical outcomes in high-risk patients hospitalized with COVID-19
1. The primary efficacy outcome of symptomatic and asymptomatic venous thromboembolism was significantly lower in the rivaroxaban group (3.14%) compared to control (9.43%).
2. No significant difference in the primary safety outcome of major bleeding was noted.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients hospitalized with COVID-19 have been suggested to have an increased risk of thromboembolic events compared to the general population. Although in-hospital thromboprophylaxis is routinely given, there is no consensus on extended thromboprophylaxis after discharge. This randomized controlled trial aimed to assess the safety and efficacy of low-dose rivaroxaban in patients at increased risk of thromboembolism post-hospitalization with COVID-19. All patients received standard doses of heparin during hospitalization and were assigned to either the rivaroxaban 10 mg/day group or no-treatment group at discharge. Venous thromboembolism (VTE) risk was assigned based on the International Medical Prevention Registry on Venous Thromboembolism (IMPROVE) score. The primary safety outcome was major bleeding, while primary efficacy outcome included a composite of VTE, arterial thromboembolism (ATE), and cardiovascular death. According to results, patients in the rivaroxaban group reported fewer instances of VTE and all-cause mortality compared to the control group at 35 days after discharge.
Click to read the study in The Lancet
Relevant Reading: Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19
In-depth [randomized controlled trial]: Between Oct 8, 2020, and June 29, 2021, 997 patients were assessed for eligibility across 14 centers in Brazil. Included were those hospitalized with COVID-19 for ≥3 days who were at increased risk of VTE. Altogether, 320 patients (160 each to rivaroxaban 10 mg/day and no anticoagulation group) were included in the final analysis. Mean patient age was 57.1 years (standard deviation [SD] 15.2) and the majority (n=191, 60%) were male. There was no difference with respect to major bleeding in either group. However, the primary efficacy outcome of symptomatic and asymptomatic DVT, and symptomatic, asymptomatic, and fatal PE, at day 35, was significantly less in the rivaroxaban group (n=5, 3.14%) compared to control (n=15, 9.43%; relative risk (RR) 0.33, 95% confidence interval [CI] 0.13-0.90, p=0.0293). Similarly, there were fewer instances of symptomatic and fatal VTE in the treatment group (n=1, 0.63%) versus control (n=8, 5.03%; RR 0.13, 95% CI 0.02-0.99, p=0.0487). Overall, this study suggests that thromboprophylaxis with rivaroxaban improves clinical outcomes in patients with hospitalized with COVID-19 and are at high-risk for VTEs.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.