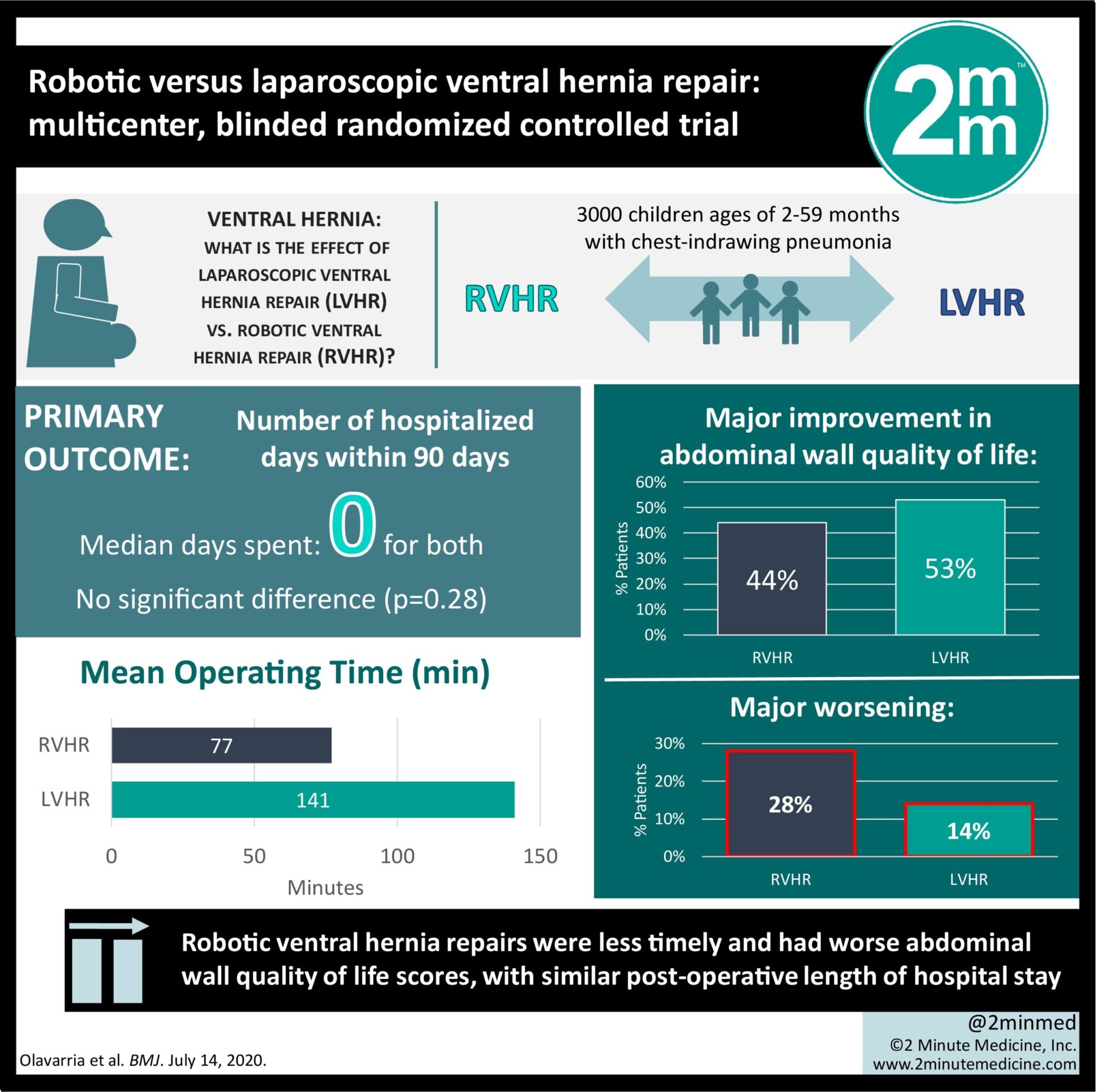
#VisualAbstract: Robotic vs. laparoscopic ventral hernia repair
1. Robotic ventral hernia repairs yielded the same post-operative length of hospital stay, but worse abdominal wall quality of life scores as laparoscopic hernia repair.
2. Robotic ventral hernia repairs were less timely and more expensive compared to laparoscopic hernia repairs.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Surgeries using robotic technologies have increased significantly in the last decade worldwide. In particular, these technologies have become more popularized in general surgery. Despite this however, the longitudinal outcomes and comparative efficacy of these surgeries are not well characterized. The current study was the first randomized controlled trial to compare patient outcomes from laparoscopic ventral hernia repair (LVHR) and robotic ventral hernia repair (RVHR). The primary outcome analyzed was length of post-op hospital stay, in which there was no difference between both groups, with a median length of stay being 0 days for both. However, LVHRs took less time to complete, were less expensive, and were associated with higher abdominal wall quality of life scores one month post-op. There was no difference in the number of complications and pain scores. As a randomized controlled trial with blinding procedures, this study represents one of the first studies to characterize outcome differences in robotic versus traditional techniques. As well, surgeries in both conditions were done by the same three surgeons for standardization. A better understanding of postoperative outcomes in robotic versus traditional techniques will allow surgeons to make more informed clinical decisions, as well as serve as potential sources of data for advancements in technique.
Click here to read the study in BMJ
In-depth [randomized controlled trial]: The study population included adults with a ventral hernia less than 12 cm wide, n = 65 for RVHR and n = 58 for LVHR. The primary outcome was the number of days a patient remained in the hospital after surgery, within 90 days of the surgery. Prior to surgery and 1 month after surgery, patients self-reported pain on a 10 point scale. They also filled out a modified Activity Assessment Scale, where a difference of 7 points is considered a minor change, and 14 points is considered a major change. The study found that the post-operative days spent in hospital were not different between both groups (p = 0.28) and the median days spent was 0 for both. The LVHRs required significantly less operating room time, with a mean±SD of 141±56 min. compared to RVHRs at 77±37 min (p<0.001). The LVHRs were significantly less expensive at $12,955±5636 compared to RVHRs at $15,865±4879. More LVHR patients had a major improvement in abdominal wall quality of life (44% vs 53%; relative risk 1.20, 0.83-1.74; p = 0.33), whereas more RVHR patients had a major worsening (28% vs 14%; relative risk 2.07, 0.98-4.41; p = 0.058). Also, the median improvement for LVHR patients was 15 points, which is a clinically significant change, whereas the median RVHR improvement was 3 points (p = 0.06). There was no significant change in pain scores, with the median being zero change in both groups (p = 0.22). Overall, these findings have implications for the cost-benefit analysis of robotic ventral hernia repairs, and in turn, their future prevalence: RVHRs are more expensive and take up more operative time, but there is no difference in post-operative hospital stay length compared to LVHRs, and a decreased abdominal wall quality of life compared to LVHRs.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.