#VisualAbstract: Roflumilast for chronic plaque psoriasis associated with clearer skin
1. A significantly greater percentage of both roflumilast groups had clear or nearly clear skin compared to the control group after 6 weeks of treatment.
2. A numerically higher number of patients in the higher-dose group achieved the primary outcome, but no statistically significant difference was detected between the treatment groups.
Evidence Rating Level: 1 (Excellent)
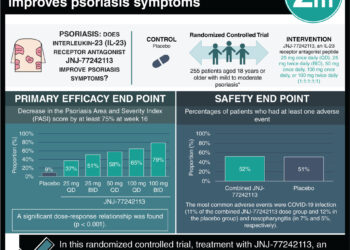
Study Rundown: Psoriasis is typically treated using topical glucocorticoids or vitamin D derivatives, but both options have significant downsides. For instance, glucocorticoids, while generally effective, are associated with slow-resolving adverse events such as cutaneous atrophy and striae distensae, and vitamin D derivatives sacrifice efficacy for safety yet still frequently cause local irritation. Phosphodiesterase type 4 (PDE-4) is involved in the regulation of numerous inflammatory mediators and has elevated activity in psoriatic skin. An oral PDE-4 inhibitor has been FDA-approved for the treatment of plaque psoriasis, but it is unclear whether topical inhibitors such as roflumilast also demonstrate substantial efficacy and safety. This double-blind phase 2b trial involving patients with psoriasis of at least mild severity was designed to evaluate the clinical profile of roflumilast at two dose levels. After 6 weeks of daily application of the topical cream, roughly three times as many patients in the roflumilast groups had clear or almost clear skin compared to the placebo group. Application-site reactions were equally common in both the active-treatment groups and the placebo group, but upper respiratory tract infection, the most common adverse event overall, occurred exclusively in the roflumilast groups. This study was limited by both a small sample size of patients with intertriginous psoriasis and a small sample size overall which precluded analysis of several secondary outcomes.
Click here to read the study, published today in NEJM
In-Depth [randomized controlled trial]: This study was conducted from September 2018 to May 2019 at 30 sites in the United States and Canada. 331 adult participants with scores of 2 or greater on the 5-point investigator’s global assessment (IGA) were randomly assigned in a 1:1:1 ratio to receive roflumilast 0.3% cream, roflumilast 0.15% cream, or vehicle (placebo) cream. Patients were excluded if they had above-normal exposure to UV radiation, were diagnosed with guttate or pustular psoriasis, or had received PDE-4 inhibitors within the previous month, among other criteria. At week 6, 28% of the patients in the roflumilast 0.3% group and 23% of those in the roflumilast 0.15% group had an IGA score of 0 or 1 (corresponding to clear and almost clear skin, respectively), compared to only 8% of those in the vehicle group (P<0.001 and P=0.004 vs. vehicle for roflumilast 0.3% and 0.15%, respectively). At week 12, this outcome was observed in 38% of the roflumilast 0.3% group, 32% of the roflumilast 0.15% group, and 16% of the vehicle group. Further, scores on the modified Psoriasis Area and Severity Index (PASI) decreased by 50% in the roflumilast 0.3% group, 49% in the roflumilast 0.15% group, and 17.8% in the vehicle group. Adjusted confidence intervals were not able to be calculated for either of these two secondary outcomes. Application-site reactions, gastrointestinal adverse events, rand psychiatric adverse events occurred at similar rates in all groups, and no meaningful between-group differences were observed in laboratory variables, electrocardiographs, or vital signs.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.




![Nanoparticle delivery of aurora kinase inhibitor may improve tumor treatment [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2016/02/20541_lores-75x75.jpg)

