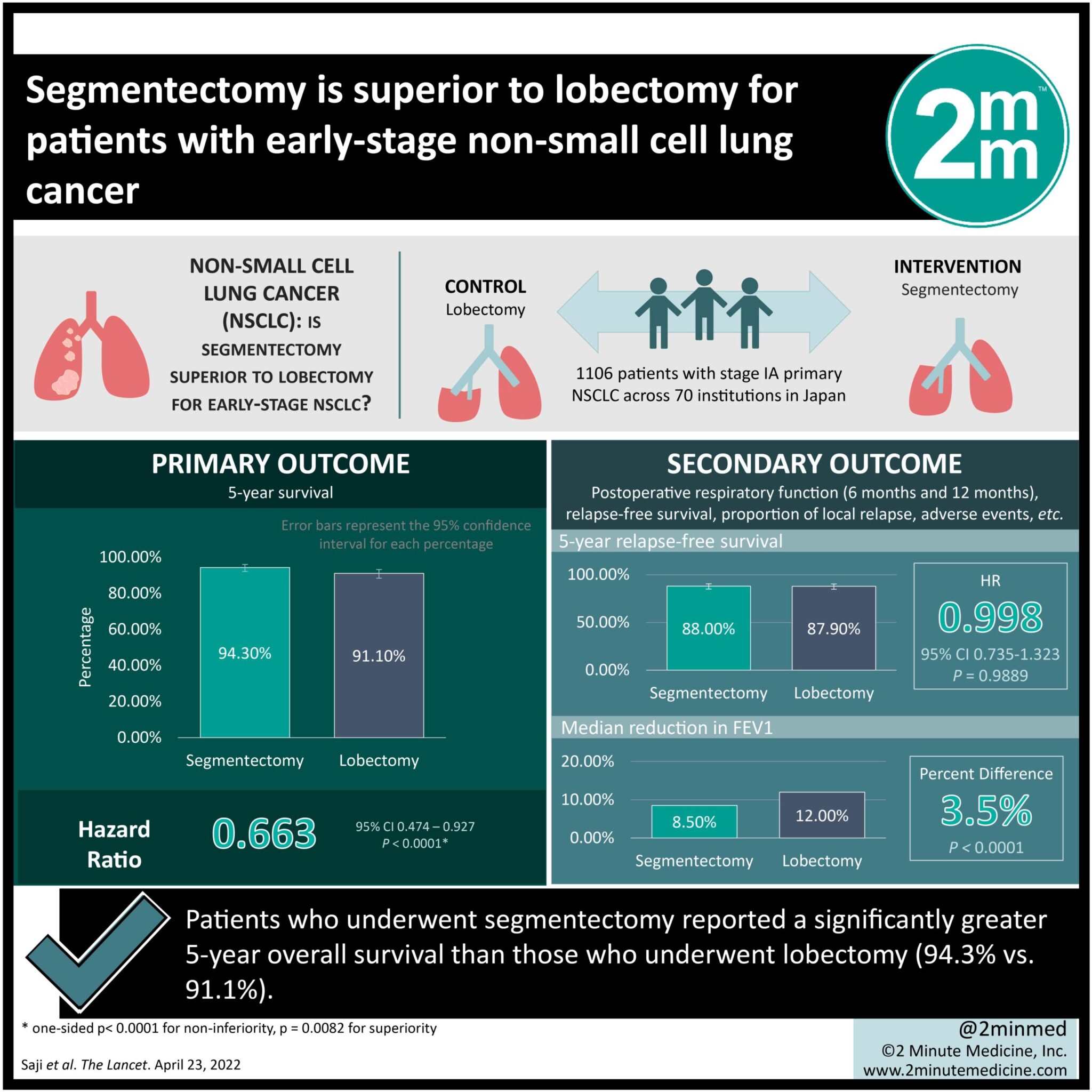
#VisualAbstract: Segmentectomy is superior to lobectomy for patients with early-stage non-small cell lung cancer
1. Patients who underwent segmentectomy reported a significantly greater 5-year overall survival than those who underwent lobectomy (94.3% vs. 91.1%).
2. Median reduction in forced expiratory volume in one second (FEV1) was greater in the lobectomy group (12.0%) compared to segmentectomy (8.5%).
Evidence Rating Level: 1 (Excellent)
Study Rundown: Surgical resection is recommended as the standard of treatment for early-stage, operative lung cancer. Lobectomy, or the surgical removal of a lobe, has been the preferred surgical modality. However, smaller tumors located in the peripheries, a less invasive option may be beneficial for long-term survival. Alternatives, such as sublobar resection or segmentectomy, can be used, although evidence around long-term prognosis is unclear. This trial aimed to compare the long-term prognosis of segmentectomy versus lobectomy among patients with primary non-small cell lung cancer (NSCLC). The primary outcome was overall survival at 5 years post-surgery, while key secondary outcomes included 5-year relapse-free survival, frequency of adverse events, length of hospital stay, and pulmonary function assessment. According to study results, segmentectomy was associated with greater overall survival and decreased all-cause mortality compared to lobectomy. There were no differences in total relapse rates between groups. This study was strengthened by a large sample size and included patients with multiple comorbidities, thus adding to validity of findings.
Click to read the study in The Lancet
Relevant Reading: Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer
In-depth [randomized-controlled trial]: Between Aug 10, 2009, and Oct 21, 2014, 1319 patients were enrolled across 70 institutions in Japan. Included were those aged ≥ 20 years with an Eastern Cooperative Oncology Group (ECOG) score of 0-1, and stage IA primary NSCLC. Altogether, 1106 patients (554 in lobectomy and 552 in segmentectomy) were included in the analysis. The primary outcome of 5-year survival was greater in the segmentectomy group (94.3%, 95% confidence interval [CI] 92.1-96.0) than in the lobectomy group (91.1%, 95% CI 88.4-93.2). The 5-year relapse-free survival was comparable in both groups (88.0%, 95% CI 85.0-90.4 for segmentectomy vs. 87.9%, 95% CI 84.8-90.3 for lobectomy; hazard ratio [HR] 0.998, 95% CI 0.735-1.323, p=0.9889). Segmentectomy was associated with a lower risk of all-cause mortality compared to lobectomy (47% vs. 63%). There was a significant difference in median reductions in FEV1 seen in patients randomized to lobectomy (12.0% at 12 months) compared to segmentectomy (8.5% at 12 months; p<0.0001). Findings from this study suggest that segmentectomy is superior to lobectomy among patients with early, stage IA, primary, non-invasive NSCLC.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.