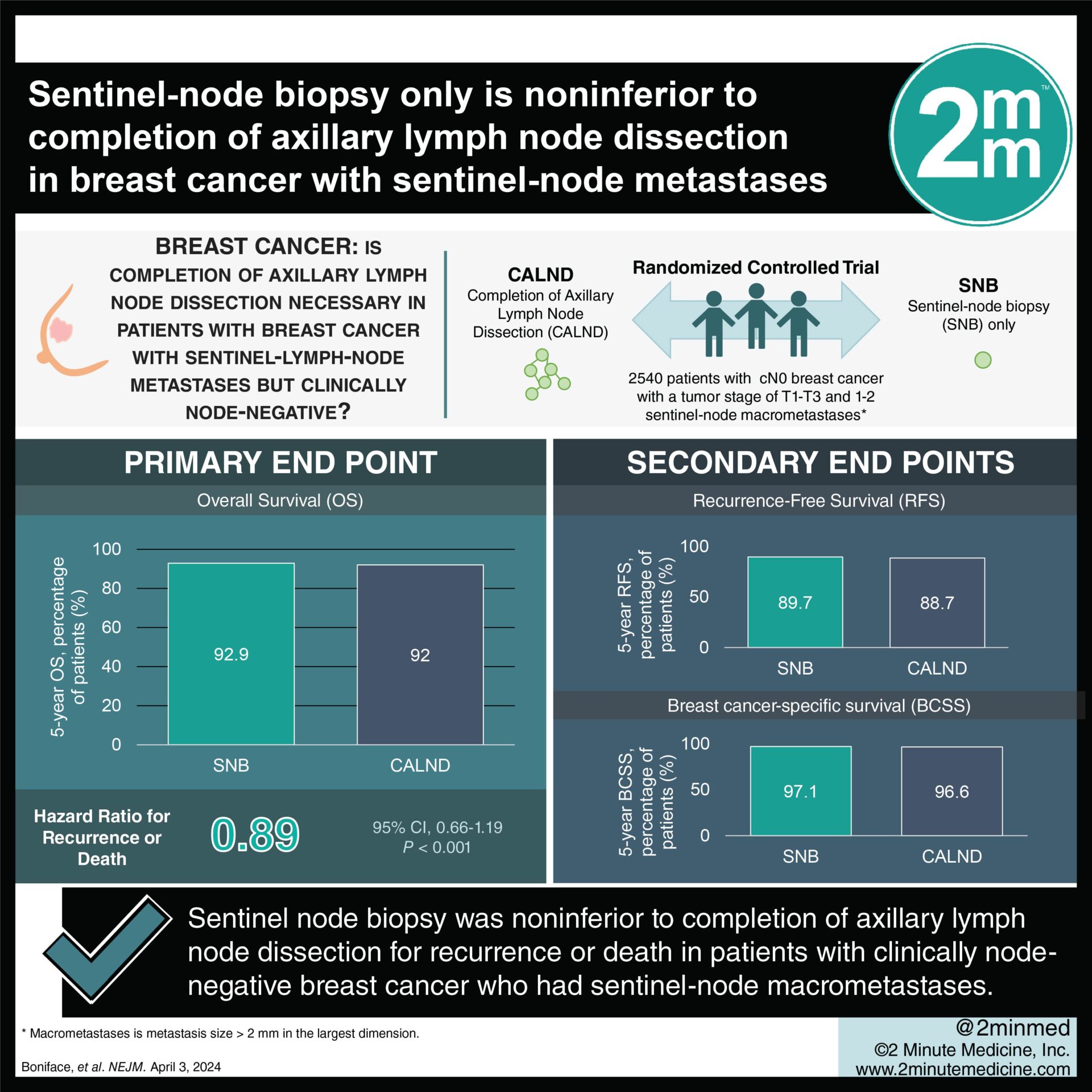
#VisualAbstract: Sentinel-node biopsy only is noninferior to completion of axillary lymph node dissection in breast cancer with sentinel-node metastases
1. The hazard ratio for recurrence or death comparing sentinel node biopsy only to completion axillary lymph node dissection was non-significant (0.89) and below the noninferiority margin.
2. The overall survival rates at 5 years were similar between both groups, 92.9% vs 92%.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Previous studies have challenged the necessity of completion axillary lymph node dissection in breast cancer treatment in certain patients. This trial aimed to validate these findings while expanding eligibility criteria. The primary endpoint was overall survival (OS), and secondary endpoints included recurrence-free survival (RFS), breast cancer-specific survival (BCSS), and patient reported outcomes. The 5-year OS was 92.9% in the SNB group and 92.0% in the CALND group. The 5-year BCSS was 97.1% in the SNB group and 96.6% in the CALND group. The 5-year RFS was 89.7% in the SNB group and 88.7% in the CALND group, with an HR of 0.89 (non-significant, p<0.001 below the noninferiority margin). Subgroup analyses were consistent with the above except in ER-positive, HER2–positive disease (13 patients total), in which SNB (HR 0.26, significant). The strength of this study included the large trial size, and the limitations included the unknown effect of differences in adjuvant therapy between the two arms. Overall, this study found that there is evidence supporting the safety of omitting CALND in patients with clinically node-negative T1-T3 breast cancer and one or two sentinel-node macrometastases.
Click to read the study in NEJM
Relevant Reading: Effect of Axillary Dissection vs No Axillary Dissection on 10-Year Overall Survival Among Women With Invasive Breast Cancer and Sentinel Node Metastasis
In-Depth [randomized controlled trial]: This multinational, prospective, randomized, phase 3 noninferiority trial, enrolled patients with T1-T3 with 1-2 sentinel node macrometastases and randomized them into completion axillary lymph node dissection (CALND, n=1205) vs no further axillary surgery (sentinel-node biopsy only, SNB, n=1335). Patients then received adjuvant radiation and systemic treatment with either hormone therapy and/or chemotherapy. The median follow-up time was 46.8 months. SNB had a mean removal of 2 lymph nodes vs CALND had a mean removal of 15 lymph nodes. The 5-year OS was 92.9% (95%CI, 91.0-94.9) in the SNB group and 92.0% (95%CI, 89.9-94.1) in the CALND group. The 5-year BCSS was 97.1% (95%CI, 95.8-98.3) in the SNB group and 96.6% (95%CI, 95.3-97.9) in the CALND group. The 5-year RFS was 89.7% (95%CI, 87.5-91.9) in the SNB group and 88.7% (95%CI, 86.3-91.1) in the CALND group, with a HR 0.89 (95%CI, 0.66-1.19, p<0.001 below the noninferiority margin). Subgroup analyses were consistent with the above except in ER-positive, HER2–positive disease (13 patients total), in which SNB (HR 0.26, 95%CI, 0.07-0.96). Overall, this study found that there is evidence supporting the safety of omitting CALND in patients with clinically node-negative T1-T3 breast cancer and one or two sentinel-node macrometastases.
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.