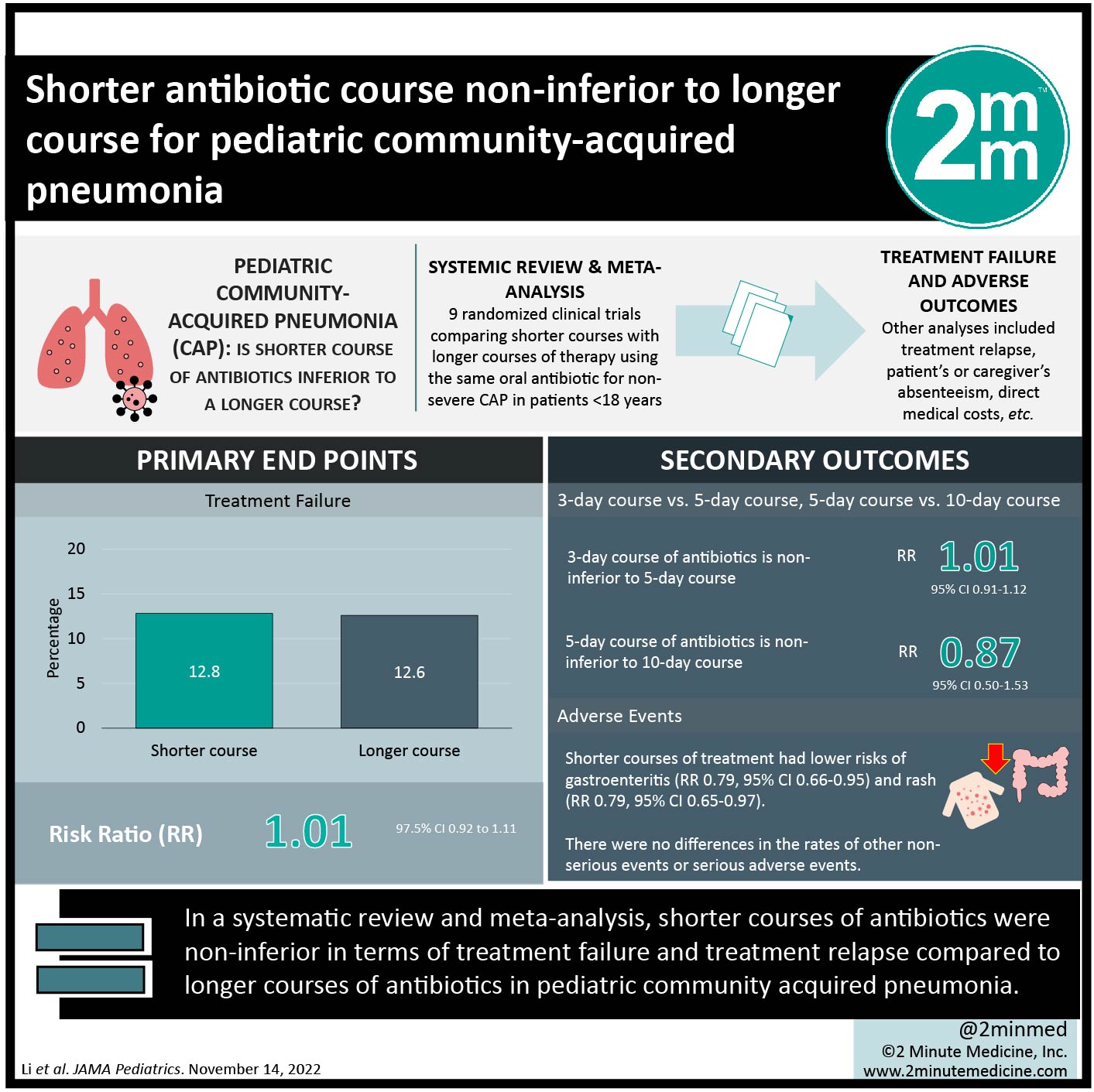
#VisualAbstract: Shorter antibiotic course non-inferior to longer course for pediatric community-acquired pneumonia
1. In a systematic review and meta-analysis, shorter courses of antibiotics were non-inferior in terms of treatment failure and treatment relapse compared to longer courses of antibiotics in pediatric community acquired pneumonia.
2. Shorter courses of antibiotics for community acquired pneumonia were associated with lower risks of non-serious adverse events such as gastroenteritis and rash compared to longer courses
Evidence Rating Level: 2 (Good)
Study Rundown: Community-acquired pneumonia (CAP) is a common infection in children, and is one of the leading causes of pediatric mortality worldwide. Limiting antibiotics to the shortest effective duration can assist with adherence and reduce adverse events. Most guidelines recommend antibiotic treatment courses of 5 to 10 days. This systematic review and meta-analysis of 9 randomized control trials (n=11,143) assessed whether a shorter course of antibiotics is noninferior to a longer course for childhood CAP. Shorter courses of antibiotics were non-inferior to longer courses in regards to treatment failure and treatment relapse. There were no differences in the rates of serious adverse events, but shorter courses of treatment were associated with a lower risk of non-serious adverse events such as gastroenteritis and rash. Limitations of this study include the small number of included studies for meta-analysis, the inability to distinguish between viral and bacterial pneumonia, and the age of subjects being mainly 12-59 months. Nonetheless, this review provides evidence that shorter courses of antibiotics should be considered in the management of non-severe pediatric CAP.
Click here to read the article in JAMA Pediatrics
Relevant Reading: Systematic review of clinical practice guidelines on the management of community acquired pneumonia in children
In Depth [systematic review]: This systematic review included all randomized clinical trials comparing shorter courses with longer courses of therapy using the same oral antibiotic for non-severe CAP in patients <18 years, with studies included from database inception to March 31, 2022. The primary outcome was treatment failure. Secondary outcomes included adverse events, treatment relapse, patient’s or caregiver’s absenteeism, antimicrobial resistance, and direct medical costs. Of the 7978 articles identified, 9 studies met inclusion criteria. Shorter course of treatment was non-inferior to longer courses for treatment failure (RR 1.01, 95% CI 0.92-1.11) and treatment relapse (RR 1.12, 95% CI 0.94-1.34). Subgroup analysis suggested that 3-day course of antibiotics is non-inferior to 5-day course (RR 1.01, 95% CI 0.91-1.12), and 5-day course was non-inferior to 10-day course (RR 0.87, 95% CI 0.50-1.53) for treatment failure. Shorter courses of treatment had lower risks of gastroenteritis (RR 0.79, 95% CI 0.66-0.95) and rash (RR 0.79, 95% CI 0.65-0.97), but there were no differences in the rates of other non-serious events or serious adverse events. The rates of antibiotic resistance were highly variable between studies. One included study suggested lower rates of caregiver work absenteeism in the 5-day course compared to 10-day group (incident rate ratio 0.74, 95% CI 0.65-0.84). In another study, mean direct medical costs of treating 1000 cases of CAP was lower in the 3-day treatment group ($1100) compared to the 5-day treatment group ($1250), although the absolute difference is minimal.
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![Oral amoxicillin as effective as injectable benzylpenicillin-gentamicin for infants with infection in which referral not possible [AFRINEST Trial]](https://www.2minutemedicine.com/wp-content/uploads/2015/04/NOVAMOXIN_antibiotic-350x250.jpg)


