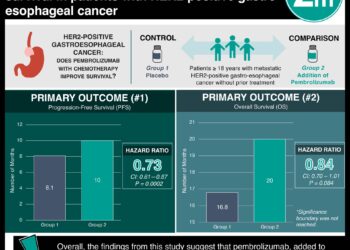
#VisualAbstract: Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912)
1. Laparoscopic-assisted distal gastrectomy is non-inferior to open distal gastrectomy for clinical stage IA and IB gastric cancer in terms of relapse-free survival at 5 year follow-up.
Evidence Rating Level: 1 (Excellent)
Laparoscopy-assisted distal gastrectomy (LADG) is now increasingly used for early stage gastric cancer, with evidence showing reduced intraoperative blood loss, lower postoperative pain, and faster recovery than open distal gastrectomy (ODG). While retrospective studies have shown equivalent survival between the two operations, LADG is technically complex and non-randomized comparative studies may be affected by selection bias in terms of operator surgical skill level. This open-label, multi-center, non-inferiority phase III randomized controlled trial aimed to compare LADG to ODG with regards to long-term relapse-free survival. Nine hundred twenty-one non-obese highly-functional (Eastern Cooperative Oncology Group [ECOG] performance status 0 or 1) adults with histologically confirmed early-stage (clinical stage I) gastric adenocarcinoma in the middle or lower third of the stomach that was amenable to curative resection were enrolled between March 2010 and November 2013. Participants were randomized to ODG(n=459) or LADG (n=462). The non-inferiority margin was established at a hazard ratio of 1.54. Of those randomized, 912 (99%) of participants had their assigned surgery. As per intention-to-treat analyses, five-year relapse-free rates were comparable between groups (94.0% [95% CI 91.4 to 95.9] vs. 95.1% [92.7 to 96.8]. Relapse free survival was similar between groups (HR 0.84, 90% CI 0.56 to 1.27). Rates of bowel obstruction, the most common serious adverse event, were similar between groups as well (2% vs. 1%). Study findings suggest that LADG is non-inferior to ODG in terms of relapse-free survival, and support LADG as standard of care over open surgery for stage I gastric cancer, alongside previous evidence supporting the efficacy and safety of laparoscopic-assisted total and partial gastrectomies in related contexts.
Click to read the study in Lancet Gastroenterology and Hepatology
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.