#VisualAbstract:Adjuvant radiotherapy does not improve survival following prostatectomy in men with localized or locally advanced prostate cancer
1. There is no evidence that adjuvant radiotherapy improves survival compared with early salvage radiotherapy following radical prostatectomy with localized or locally advanced prostate cancer.
2. Pre-surgical PSA, Gleason score, seminal vesicle involvement and surgical margins did not influence the effect of adjuvant radiotherapy on event-free survival.
Evidence Rating Level: 1 (Excellent)
Study Rundown: There is a lack of consensus in current guidelines on whether adjuvant or early salvage radiotherapy is more appropriate following prostatectomy in patients with localized or locally advanced prostate cancer. Prior randomized trials have showed adjuvant radiotherapy to result in better biochemical control compared to observation but did not show a consistent benefit for long-term survival outcomes. Thus, the recommendation of adjuvant radiotherapy in clinical practice has been questioned. This systematic review and meta-analysis utilized a prospective framework for adaptive meta-analysis (FAME) to include three randomized controlled trials comparing immediate adjuvant radiotherapy versus early salvage radiotherapy men following radical prostatectomy with localized or locally advanced prostate cancer. Results showed no evidence that use of adjuvant radiotherapy following prostatectomy improved PSA-driven event-free survival in men with prostate cancer. Additionally, there was no evidence that the effectiveness of adjuvant radiotherapy varied based on pre-surgical PSA, Gleason score, seminal vesicle involvement or surgical margins. A notable strength of the study includes the utilization of a prospective FAME approach to work closely with trialists to limit bias both in study selection and in the analysis through harmonizing key survival outcome definitions and allowed for the planning of analysis prior to the final trial results being known. The absence of individual participant data during the study period necessitated the adoption of an aggregate data approach and therefore insufficient power to detect a very small (<5%) benefit of early radiotherapy.
Click to read the study in The Lancet
In-Depth [systematic review]: This systematic review and meta-analysis of aggregate data utilized a prospective framework for adaptive meta-analysis (FAME) approach to include three ongoing trials recruiting men (age >18 years) with localized or locally advanced prostate cancer who had radical prostatectomy prior to trial enrolment. Trials included were aimed to compare adjuvant radiotherapy to a policy of deferred, early salvage radiotherapy following radical prostatectomy. The primary outcome measure at this initial stage of the meta-analysis was event-free survival with all included trials utilized a harmonized definition of this outcome with identical endpoints.
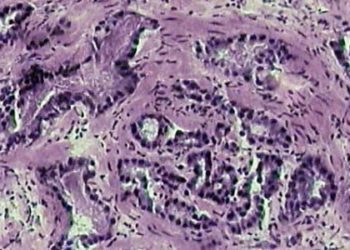
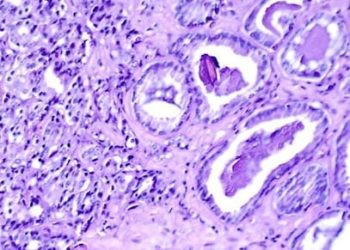
A total of 2153 patients (median age 64-65 years; 1075 randomized to receive adjuvant radiotherapy)) were included in the aggregate data analysis with median follow-up ranging from 60 to 78 months. Most patients had a Gleason score of 7 (1671 patients, 77.6%), positive surgical margins (1526 patients, 70.9%), either stage pT3a or b disease (1719 patients, 79.8%) and extracapsular extension (1656 patients, 76.9%). Of the 270 events recorded, there was no evidence that event-free survival was significantly improved with adjuvant radiotherapy compared to early salvage radiotherapy (hazard ratio (HR) 0.95, 95% CI 0.75 to 1.21; p=0.70) with results being consistent across trials (heterogeneity p=0.18 I2=42%). The baseline event-free survival rate was 88% at 5 years with a 1% absolute difference between early salvage radiotherapy and adjuvant radiotherapy (95% CI -2 to 3). There was no evidence that event-free survival following adjuvant radiotherapy varied based on predefined subgroups including pre-surgical PSA, Gleason score, seminal vesicle involvement or surgical margins.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.